Click here
to go to our new blog!
Stony Brook Surgery Blog
Posted by Stony Brook Surgery on September 17, 2019
Posted by Stony Brook Surgery on September 4, 2019
We Know How to Help Kids Achieve a Healthy Weight and Stay That Way

| We must recognize the problem and do everything we can to solve it. |
Childhood obesity keeps growing at an epidemic rate, along with that of adults.
More than one-third (40%) of U.S. adults have obesity, according to the latest numbers provided by the Centers for Disease Control. Nationwide, nearly 14 million children and adolescents aged 2 to 19 are obese.
Nearly one-fifth of kids are obese. How terribly sad! The obesity prevalence is around 14% among 2- to 5-year-olds, 18% among 6- to 11-year-olds, and 21% among 12- to 19-year-olds.
Since 1980, the childhood obesity rates (ages 2 to 19) have tripled — with the rates of obese 6- to 11-year-olds more than doubling (from 7% to 18%) and rates of obese adolescents (ages 12 to 19) quadrupling from 5% to 20%.
Childhood obesity is a condition where excess body fat negatively affects a child's health or well-being. As methods to determine body fat directly are difficult, the diagnosis of obesity is often based on body mass index, known as BMI. (Click here to use the CDC online BMI calculator for children.)
One out of five children in the United States has obesity now — and that's cause for alarm.
In Suffolk County alone, there are more than 5,000 obese students in middle and high school.
Obese children often have adult diseases, such as type 2 diabetes, high blood pressure, and heart disease, because of their extra body weight. In such cases, treatment becomes more urgent.
Stony Brook Children's multidisciplinary Healthy Weight and Wellness Center is dedicated to providing a range of treatment options, from diet change to surgery performed by our bariatric specialists.
Commenting on obesity in adolescents and the benefit of bariatric surgery, Konstantinos Spaniolas, MD, associate professor surgery and associate director of our Bariatric and Metabolic Weight Loss Center, says:
"Obesity and associated diseases (metabolic, psychologic, orthopedic, etc.) have a deleterious effect in adolescents with severe future cardiovascular risks. It is likely that an early intervention in this age group can disrupt the progression of disease, and lead to long-lasting benefit.
"Recent published evidence demonstrates profound and sustained weight loss in adolescents that is maintained at least 3 years after metabolic surgery. Importantly, 95% of adolescents with type 2 diabetes experience lasting remission at 3 years."
At present, weight loss surgery provides the only effective, lasting relief from severe obesity.
Obesity most commonly begins between the ages of 5 and 6, or during adolescence. Studies have shown that a child who is obese between the ages of 10 and 13 has an 80% chance of becoming an obese adult.
Obesity increases the risks of morbidity and mortality because of the diseases and conditions that are commonly associated with it, such as type 2 diabetes, hypertension, and cardiovascular disease, among other health risks.
Therefore, the American College of Surgeons believes it is of utmost importance to extend its quality initiatives to accrediting bariatric surgery centers so that it can assist the public in identifying those facilities that provide optimal surgical care for patients who undergo this surgical procedure.
In 2014, Stony Brook Medicine was first granted full accreditation as a comprehensive bariatric facility by the MBSAQIP, then a newly established program of the American College of Surgeons and American Society of Metabolic and Bariatric Surgery.
Every member of our large multidisciplinary team is committed to our program, and this commitment is the key of our success. We are all extremely proud of the work we do, and proud of our continued recognition by the MBSAQIP.
Our mission is to help children and adults who have issues with too much extra weight to achieve a healthy weight and stay that way.
| Individualized assessment and care are crucial for the long-term success of weight loss treatment. At Stony Brook Medicine, our bariatric specialists welcome any pediatric/adolescent patient over the age of 12 for evaluation. With the close involvement of specialized pediatricians, dieticians, and psychologists, a thorough assessment of patient and family allows for proper guidance. We offer the full gamut of weight loss options, and many patients will be successful with lifestyle and behavioral modification alone. Bariatric surgery or other interventions are sometimes offered to further assist with weight loss and control of co-existing medical problems. |
For consultations/appointments with our bariatric specialists, please call 631-444-BARI (2274) . Watch the News 12 L.I. video (2:47 min) of the weight loss story of a teenager treated by our team:
Posted by Stony Brook Surgery on August 29, 2019
An Emotional Story with a Happy Ending at Stony Brook Children's

| East Patchogue teen Thomas Spiotta with big smile as he was wheeled out of Stony Brook Children's Hospital and greeted by 50 of his fellow North Patchogue firefighters. Standing behind him were Dr. Christopher S. Muratore (left) with his family. Click on photo to enlarge it. |
The headlines of various local and regional media spread the news of this highly emotional story with a happy ending, which took place at Stony Brook Children's Hospital:
"Tommy Spiotta Battled Back and His Firefighter Family Cheered Their Support" (Newsday), "East Patchogue Teen, Volunteer Firefighter Survives Life-Threatening Blood Clot" (News 12), "LI High Schooler Fighting Rare Illness Leaves Hospital" (NBC), "Teen with Down Syndrome Comes Home to Fanfare after Health Scare (Patchogue Patch).
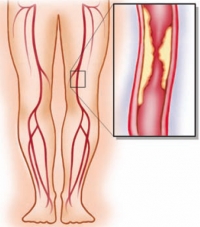
Christopher S. Muratore, MD, chief of pediatric surgery, and his team at Stony Brook Children's performed a series of three operations to save the life of 19-year-old Thomas Spiotta who had developed life-threatening blood clots in his portal vein, the blood vessel that carries blood from the gastrointestinal tract, gallbladder, pancreas, and spleen to the liver.
"The portal vein is one of the major veins bringing blood back from all of the intestines to the liver," Dr. Muratore explains.
Our surgeons may not be divine, but they provide the highest possible level
of pediatric surgery at Stony Brook Children's.
Because of the clots, the young man's intestines began to die. To save him, Dr. Muratore and his team performed three major operations, removing about three feet of intestines.
"We identified the major veins with the clot in it, and we opened up the vein to remove the clot, then used a clot-busting medication to help restore some of the blood flow," says Dr. Muratore.
After seven weeks of hospitalization, the patient was discharged on Tuesday, August 27. He was greeted by a cheering crowd of fellow firefighters as he left the hospital.
Before the departure, a press conference took place where the patient's mother said she believed her son had been saved by a miracle. Our surgeons may not be divine, but they provide the highest possible level of pediatric surgery at Stony Brook Children's.
Check out the story on some of the various local and regional media that covered it:
- Newsday video (subscription may be needed)
- Newsday article (subscription may be needed)
- News12 (long video)
- News12 (short video)
- FiOS1 (short video)
- NBC (short video)
- Patchogue Patch
- Greater Patchogue
Posted by Stony Brook Surgery on August 22, 2019
First on Long Island to Offer Dialysis Patients EndoAVF
There are more than 440,000 Americans with end-stage renal disease (ESRD), the final stage of kidney failure. When a patient has ESRD, their kidneys are no longer able to keep up with the body's need to remove excess waste and water.
In fact, once kidney function goes below 10-15% of normal, hemodialysis — the process of removing fluid and toxins from the blood via an artificial kidney machine — is necessary for survival.
Linking to the bloodstream is crucial in administering dialysis treatment to these patients.
For over 50 years a surgically created artery-vein fistula (AVF) — a connection between an artery and a vein — has been the standard of care to achieve vascular access for dialysis patients.
Until now.
The FDA in August 2018 approved a less invasive alternative to the traditional surgery: endovascular artery-vein fistula (endoAVF), also called percutaneous (through/under the skin) fistula.
We are leading the way in patient care with leading-edge technology and our advanced endovascular skills.
The Stony Brook Vascular Center is the first on Long Island to offer dialysis patients endoAVF.
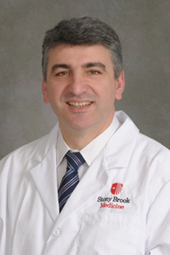
Apostolos K. Tassiopoulos, MD, professor of surgery and chief of vascular and endovascular surgery, and director of the Stony Brook Vascular Center, says
"EndoAVF is a minimally invasive alternative to the traditional surgically created AVF which requires detailed planning to determine if a specific patient is an appropriate candidate.
"Therefore, it is particularly important to have not only a group of surgeons with expertise in hemodialysis access and advanced catheter and wire skills, but also skilled vascular lab technologists and nurses focusing on patient education to help maximize procedural success.
"Only a small number of institutions including our own currently have this type of advanced diagnostic and interventional expertise, together with the specialized training component required to perform endoAVF.
"Stony Brook University Hospital is among the first vascular centers in the nation, and the first on Long Island, to offer this innovative technology to benefit our patients."
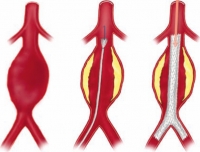
In a traditional AVF procedure, the fistula is created by making a surgical incision, usually in an arm, repositioning a superficial vein from adjacent tissues, and then sewing together the vein onto a nearby artery, thus creating a high blood flow shunt.
An endovascular AV fistula is instead created using minimally invasive catheters that utilize electro-magnetic waves to create the channel between the vein and artery. This approach leaves minimal scarring from the fistula creation procedure.
EndoAVP benefits are quicker recovery time, plus less infection risk, pain, scarring, and arm disfigurement.
In one preliminary study, the usability (maturation) of the percutaneously placed AVF was 95-96%, while for a surgically created AVF, usability was just 75% or less," says Dr. Tassiopoulos.
"If a patient has the relevant anatomy, then there is definitely what's considered an early advantage. The procedure takes no more than an hour and a half, the maturation process takes five to six weeks, and the maturation rate is about 95%."
In addition to Dr. Tassiopolos, our vascular specialists providing endoAVF are Mohsen Bannazadeh, MD, and Angela A. Kokkosis, MD.
About the Procedure
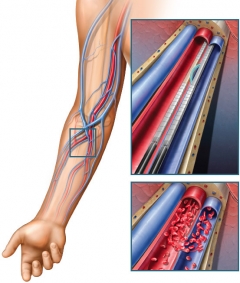
| Vascular access created with endoAVF procedure. Top inset shows magnets on catheters pulling artery and vein together (pressure), followed by application of radiofrequency (heat) which makes hole between the two to create artery-vein fistula, shown in bottom inset (click on image to enlarge). |
The endoAVF procedure requires only two small micro-punctures in the arm. Two thin, flexible magnetic catheters (tubes) are inserted into an artery and vein under x-ray guidance.
The artery and vein access location may include the upper arm (brachial artery/vein) or the forearm above the wrist (ulnar vein or radial vein).
Once the desired site is reached (usually between two vessels within close proximity to each other), a small burst of electro-magnetic energy — heat — between the two catheters is used to create the fistula.
The catheters are then removed.
The AVF can be used for hemodialysis after a healing time of around six weeks with the endoAVF procedure. Recovery time can be significantly shorter than with open surgery, as there is less trauma to the area.
Once the fistula is healed and mature, high blood flow allows blood to be withdrawn, cleaned through the dialysis machine, and returned to the body.
People living with ESRD are an underserved patient population with very limited treatment options available to them. With endoAVF the Stony Brook Vascular Center is leading the way in patient care with leading-edge technology together with advanced vascular skills.
| "The data available so far present endoAVF as the most encouraging and exciting development in arteriovenous access in 50 years. EndoAVF has the potential to provide an extended lifeline requiring much lower maintenance and morbidity than the traditional AV access in end-stage renal failure patients…. Local expertise will probably determine who will be the main operators in endoAVF creation." — "A Review of the Current Status of Percutaneous Endovascular Arteriovenous Fistula Creation for Haemodialysis Access, " Cardiovascular and Interventional Radiology (2019) |
Posted by Stony Brook Surgery on August 21, 2019
The surgical robot made its debut in the late 1990s, and it is increasingly used to perform a wide range of operations, including procedures to treat different cancers.
Now, surgeons are using robotic technology to expand their technical surgical capabilities.
Robotic systems are equipped with multiple robotic arms that surgeons control precisely using a nearby high-tech surgeon console.
One robot arm utilizes a small video camera with 3-D optics and visualization. The other three robotic arms utilize specialized surgical instruments that can access the surgical field through incisions each less than an inch long.
The surgeon sits at the console with a screen providing enhanced 3-D visualization of the operative field.
Hand controls that are similar to those used in video games allow surgeons to control the bed-side robotic instrumentation, providing them with full wrist dexterity and hand movements with a minimally invasive approach to enhance surgical precision.
Like other surgical methods and technologies, robotic surgery offers a variety of benefits for both patients and surgeons.
In 2017, our surgical oncologists at the Stony Brook Cancer Center performed Long Island’s first totally robotic Whipple procedure for pancreatic cancer, advancing patient care significantly.
Here, Sherif R. Abdel-Misih, MD, a member of our Surgical Oncology Division with extensive experience and expertise in robotic surgery as well as a range of other surgical expertise, answers frequently asked questions about robotic surgery for cancer treatment.
Q: What is robotic surgery?
A: Robotics is a surgical technology platform first and foremost used by surgeons to enhance surgical capabilities.
Q: Does the robot perform the surgery alone, or does the surgeon perform the surgery?
A: The operating surgeon is in control of the technology and the conduct of the operation. I not uncommonly joke with my patients but clarify that I don’t simply flip the switch and go play a round of golf. I am the one performing the surgery.
Q: What cancers are currently treated with robotic surgery?
A: Robotic technology has allowed many disciplines to incorporate robotic surgery into their operative management of many cancers, including lung, esophagus, gynecologic (ovarian, endometrial), urologic (kidney, bladder, testicular), and gastrointestinal cancer (stomach, pancreas, colorectal), to name some.
Robotic surgery has improved patient recovery, specifically pain, time in the hospital,
and return to everyday life and activities.
Q: What are the benefits of robotic surgery compared to traditional (open) methods of surgery?
A: Minimally invasive surgery done with robotics has improved patient recovery from surgery, specifically pain, time in the hospital, and return to everyday life and activities. Also, in many cases, robotic surgery allows the surgeon to achieve a higher degree of precision due to the enhanced dexterity and 3-D visualization provided by the robotic system.
I myself found these advantages very useful from my early experience now more than eight years ago when I began utilizing this technology to assist in the surgical management of patients with rectal cancer who I cared for. As I expanded robotic utilization to other cancers I treated, these advantages were further demonstrated to be of benefit.
Q: Is robotic surgery safe? What are its risks, in any, in cancer treatment?
A: In experienced hands, robotic surgery is safe because it is a technology like others that has to be used appropriately to achieve the desired surgical goals and outcomes. All surgeries carry some degree of risk.
Q: Why is the number of robotic surgeries performed important in choosing a surgeon?
A: Experience is important in all facets of life, and the greater the experience and exposure to a technology or surgical approach, the more skilled one becomes.
Q: What makes a patient a good candidate for robotic surgery?
A: Candidacy for surgery relates to the feasibility, safety, and quality of an operation that can be undertaken with any surgical approach or technology.
There are conditions and cancers that are sometimes too technically challenging or risky to reasonably substantiate a less invasive approach using robotic technology. However, by and large, in experienced hands, many patients will benefit from minimally invasive surgical approaches using robotic technology by enhancing or improving their recovery.
Stony Brook cancer specialists with expertise in robotic surgery have years of experience,
and are leaders in the field of robotics.
Q: Is robotic surgery covered by insurance?
A: Yes. Insurances generally cover use of the robotic platform because it is a technology and approach to surgery still directed at traditional problems and operations.
Q: What is the advantage of having robotic surgery for cancer treatment done at Stony Brook Cancer Center?
A: Robotic surgical approaches are being used by many of our surgical disciplines with increasing frequency, which continues to enhance our experience and expertise. The outstanding operating room team support given our surgeons is a major asset. Together, our robotics focus and team approach provide for high-quality surgical care and outcomes.
The surgeons on the Cancer Center's Gastrointestinal Oncology Team who perform robotic surgery have years of experience, and are leaders in the field of robotic surgical oncology. We are committed to using robotics to make leading-edge surgeries a reality, as we did with Long Island's first totally robotic Whipple procedure for pancreatic cancer.
| Use of the surgical robot allows operations for cancer treatment to be performed accurately and in a more minimally invasive way. At Stony Brook, increasing numbers of patients with cancer are being treated with surgery using robotics, and are benefiting from this advance in care. |
Posted by Stony Brook Surgery on August 14, 2019
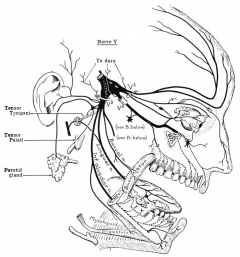
The trigeminal nerve — the fifth cranial nerve — is a complex nerve responsible for sensation in the face and motor functions such as biting and chewing.
The trigeminal nerve is the largest of the cranial nerves that emerge directly from the brain, in contrast to spinal nerves.
The several branches of the trigeminal nerve supply sensation to the upper face, midface, upper lip, jaw and palate, lower face, lower lip, and tongue.
These trigeminal nerve branches can be injured by facial trauma, local anesthesia, or surgical procedures, and lose their function. Complete sensory recovery from such injuries seldom occurs spontaneously.
Peripheral trigeminal nerve injuries can result in permanent sensory dysfunction, such as decreased or lost sensation, painful sensation, or a combination of both.
This sensory dysfunction in the face and/or mouth often interferes with performance of activities of daily living, and may adversely affect the lives of afflicted patients.
Microsurgical repair of trigeminal nerve injuries can achieve functional
sensory recovery and restore quality of life.
In selected patients, microsurgical repair of trigeminal nerve injuries can be helpful in achieving functional sensory recovery and in improving quality of life.
Few surgeons are trained or provide this surgery. But at Stony Brook Medicine, we have David K. Lam, MD, DDS, PhD, professor of surgery and chief of oral and maxillofacial surgery.
Here, Dr. Lam regularly performs this very complex microsurgical repair procedure, which can potentially restore lost feeling in the face and mouth.
Dr. Lam treats patients who endure trigeminal nerve injuries from trauma, head and neck cancer surgery, oral and maxillofacial surgery, and dental procedures (usually following implants or wisdom teeth removal).
"Advances in microsurgical techniques and materials," says Dr. Lam, "have improved our ability to manage these injures, and have also expanded the applications of micro-neurosurgery, resulting in excellent success rates."
The patient with a trigeminal nerve injury may experience a variety of distressing sensations, such as numbness, tingling, burning, or hypersensitivity of the affected area.
Sensations like these due to trigeminal nerve injuries may interfere with normal speaking, chewing, drinking, eating, shaving, or kissing. Their impact on quality of life is often very negative.
Ideally, persistent symptoms of trigeminal nerve injuries are addressed early
in order to prevent irreversible damage.
When these sensations persist for months following the initial nerve injury, the chance the injury won't resolve by itself is high. That's why early evaluation by a specialist for management and treatment is indicated.
Initial care of trigeminal nerve injuries involves close monitoring of symptoms and neurosensory testing.
The best time to treat a trigeminal nerve injury with surgical repair is controversial but is ideally within three months of the initial injury. This time frame is associated with the highest rate of success.
The specialized microsurgical techniques used by Dr. Lam improve the healing of nerves, thus providing a better chance for recovery of sensation.
Ideally, patients or their doctors will identify the symptoms of trigeminal nerve injuries early, and will address the injuries that don't resolve by themselves, in order to prevent irreversible damage.
The microsurgical repair of trigeminal nerve injuries, in Dr. Lam's hands, usually takes 3-4 hours with the patient under general anesthesia. Usually no overnight hospitalization is required.
The procedure is usually performed through the mouth, so there is no visible scar.
Recovery from the procedure generally takes 7-10 days, at which time patients can return to their normal activities.
| "My unique multidisciplinary experience and training in medicine, dentistry, anesthesia, neurophysiology, and surgery allow me to ensure optimal care for patients with evidence-based and solutions-focused management, as well as innovative therapies, including the latest in the microsurgical repair of trigeminal nerve injuries." — Dr. David K. Lam |
Posted by Stony Brook Surgery on August 1, 2019
August is National Gastroparesis Awareness Month. First listed on the U.S. National Health Observances Calendar in 2016 with sponsorship by the International Foundation for Functional Gastrointestinal Disorders, this awareness initiative aims to focus attention on diagnosis, treatment, and quality of life issues associated with this poorly understood motility condition that prevents the stomach from properly emptying.
Gastroparesis, or delayed gastric emptying, is a stomach disorder in which food moves through the stomach into the intestines slower than normal. (The etymology of "gastroparesis" is: gastro- from ancient Greek γαστήρ gaster, "stomach" and πάρεσις -paresis, "partial paralysis.")
Patients often experience chronic nausea, vomiting, bloating, feeling full too soon after starting to eat, and weight loss. It is a debilitating condition, at times requiring hospitalization, and can significantly affect a person's quality of life.
Common causes include diabetes and previous surgery. Diabetes has been noted to be a cause in 30% of gastroparesis cases. However, neurological disease, collagen vascular disorders, viral infection, and drugs have all been blamed.
The Stony Brook Gastroparesis Center offers state-of-the art treatment.
Gastroparesis is believed to occur in 9.6 per 100,000 people in men and 37.8 per 100,000 people in women. A recent study has also demonstrated an increase in gastroparesis-related hospital admissions by nearly 300% over a 16-year period.
The rising prevalence of gastroparesis, especially among children and minority groups, might be associated with the rise in diabetes, according to the authors of an epidemiological study published this year (see abstract).
Gastroparesis may result in the following complications, which, in addition to potentially problematic symptoms, justify treatment:
- Severe dehydration: This condition is due to chronic vomiting.
- Malnutrition: Patients tend to have poor appetites and cannot meet their daily caloric requirements.
- Poor glucose control: Poor control over the amount and rate of food passing from the stomach to the small bowel can cause poorly controlled blood sugar levels.
- Poor quality of life: Symptoms can make it difficult to maintain a normal quality of life and may affect a patient's work and social life.
Gastroparesis, if not cured, requires management with a long-term care plan.
The Stony Brook Gastroparesis Center, established in 2018 under the direction of Salvatore Docimo Jr., DO, MS, offers a multidisciplinary approach that brings together experts in the areas of surgery, gastroenterology, psychology, and nutrition.
Our center's goal is to provide patients with digestive disorders, especially gastroparesis, a wide spectrum of diagnostic and treatment options under one roof.
Last year, Dr. Docimo performed Suffolk County's first per-oral pyloromyotomy (POP) — a novel, minimally invasive procedure to treat gastroparesis.
Now at the forefront of gastroparesis treatment, the POP procedure (also known as G-POEM that stands for gastric per-oral endoscopic myotomy) is a newly developed treatment offering patients attractive benefits, compared with other surgical therapies for gastroparesis.
It was in July 2016 that U.S. Senator Tammy Baldwin (WI) introduced a statement for the record on behalf of the millions of Americans affected by gastroparesis recognizing National Gastroparesis Awareness Month.
Senator Baldwin said: "Unfortunately, gastroparesis is a poorly understood condition, and so patients often suffer from delayed diagnosis, treatment, and management of this disorder. As such, further research and education are needed to improve quality of life for this patient population."
Senator Baldwin urged her fellow colleagues to join her "in recognizing August as National Gastroparesis Awareness Month in an effort to improve our understanding and awareness of this condition, as well as support increased research for effective treatments for gastroparesis" (read her entire statement).
She succeeded in Congress, and so August now is National Gastroparesis Awareness Month, a good time to learn about this poorly understood motility condition affecting millions and apparently on the rise.
| The Stony Brook Gastroparesis Center, under the direction of Dr. Salvatore Docimo Jr., offers a multidisciplinary approach that brings together experts in the areas of surgery, gastroenterology, psychology, and nutrition. The center's goal is to provide patients with digestive disorders, especially gastroparesis, a wide spectrum of diagnostic and treatment options under one roof. |
Posted by Stony Brook Surgery on July 12, 2019
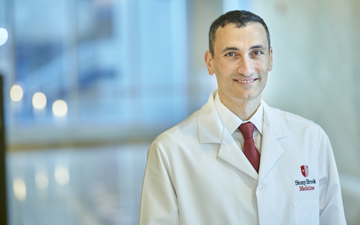
We are very pleased to spotlight Henry J. Tannous, MD, the new chief of our Cardiothoracic Surgery Division and co-director of the Stony Brook Heart Institute.
Dr. Tannous was appointed in April to these key leadership roles in recognition of his expertise, accomplishments, and outstanding reputation for clinical excellence in both adult cardiac and thoracic surgery.
"I am very honored by my new appointments at Stony Brook Medicine, as well as excited to lead my division to even greater heights," says Dr. Tannous.
"My talented and accomplished colleagues here are the perfect team, each complementing the other in terms of surgical skills and academic prowess. Our clinical support staff is first-rate. Together, I believe we will maintain our rank as the very best on Long Island.
"The Stony Brook Heart Institute will continue to expand patient access across Long Island while maintaining the best outcomes and driving innovation to further enhance patient care."
Recognized early in his career as a physician of the highest order, Dr. Tannous received his MD from the American University of Beirut in 2000, graduating as a member of the Alpha Omega Alpha Medical Honor Society.
He went on to complete his general surgery residency at Waterbury Hospital-Yale School of Medicine in Waterbury, CT, in 2005. He subsequently completed fellowships in cardiothoracic surgery at George Washington University and Mount Sinai Hospital.
"My talented and accomplished colleagues here are the perfect team,
each complementing the other in terms of surgical skills and academic prowess.
Our clinical support staff is first-rate."
Dr. Tannous then joined the faculty at the Icahn School of Medicine at Mount Sinai in 2008, where he distinguished himself as a clinical and team leader.
At Mount Sinai, he served as chief of pump-assisted thoracic surgery, chief of the cardiothoracic expansion program, and chief of thoracic surgery at St. John's Riverside Hospital in Yonkers, NY.
Dr. Tannous was recruited to Stony Brook University Hospital from Mount Sinai in 2016, serving as surgical director of the structural heart program and associate chief of the Cardiothoracic Surgery Division.
He has been instrumental in major Stony Brook Medicine milestones, including the top national three-star rating for coronary bypass surgery earned two years in a row; the remarkable successes of our transcatheter aortic valve replacement (TAVR) program; and fostering successful clinical collaborations with our key partners across the community and regionally.
Dr. Tannous's clinical practice encompasses coronary revascularization and valvular heart surgery, including transcatheter interventions and minimally invasive lung cancer surgery.
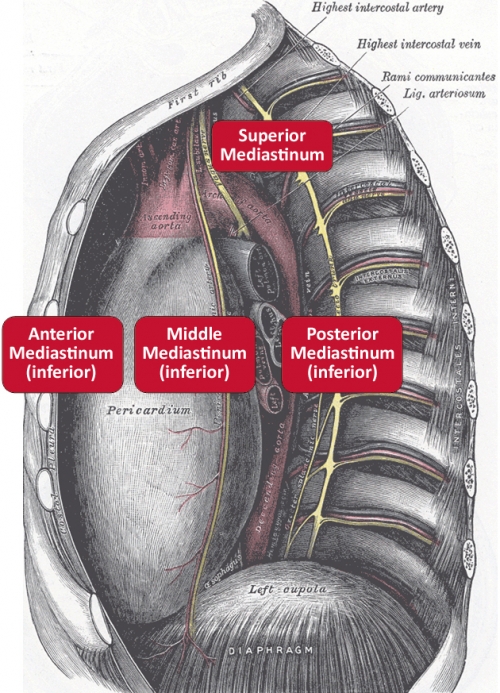
He has additional experience in pump-assisted thoracic procedures supporting more aggressive resection of mediastinal tumors, cardiac tumors, and locally advanced lung tumors.
His research focuses on early-stage treatment of lung cancer, with the goal of reducing lung cancer death rates through early detection and treatment through a Stony Brook collaboration with the International Early Lung Cancer Action Program; and comparative outcomes research in TAVR.
Dr. Tannous is dual board certified by the American Board of Surgery and the American Board of Thoracic Surgery.
Posted by Stony Brook Surgery on July 10, 2019
Recognition of Our Focus on Continuous Improvement of Patient Care

| Our vascular faculty: (left to right) Drs. Nicholas Sikalas, Shang A. Loh, David S. Landau, Apostolos K. Tassiopoulos, Angela A. Kokkosis, Antonios P. Gasparis, Nicos Labropoulos, and Mohsen Bannazadeh (click on photo to enlarge). (Not pictured is George J. Koullias.) |
The Society for Vascular Surgery's Vascular Quality Initiative (SVS VQI) has just awarded Stony Brook Medicine three stars — the top rating — for its active participation in the Registry Participation Program.
The SVS VQI registry provides real-time data and gives opportunities for vascular surgery-related quality improvement projects.
The mission of the SVS VQI is to improve patient safety and the quality of vascular care delivery by providing web-based collection, aggregation and analysis of clinical data submitted in registry format for all patients undergoing specific vascular treatments. The VQI operates 12 vascular registries.
The participation awards program began in 2016 to encourage active participation in the registries program and recognize the importance of that participation.
Participating centers can earn up to three stars based on actions that lead to better patient care, including:
- The completeness of long-term, follow-up reporting, based on the percentage of patients for whom they have at least nine months of follow-up data.
- Physician attendance at semi-annual meetings of a regional quality group.
- Initiation of quality improvement activities based on VQI data.
- The number of vascular registries in which the center participates.
"This second year in a row 3-star level designation is an acknowledgment of
our focus on continuous improvement in the care of our patients."
VQI's registries contain demographic, clinical, procedural, and outcomes data from more than 500,000 vascular procedures performed in the U.S. and in Canada. Each record includes information from the patient's initial hospitalization and at one-year follow-up.
The wealth of data allows centers and providers to compare their performance to regional and national benchmarks. All centers and providers receive biannual dashboards and regular performance reports, so they can use their data to support quality improvement initiatives.
Our vascular care team at the Stony Brook Vascular Center uses VQI data to measure the effectiveness of our programs and to improve our long-term patient care.
Apostolos K. Tassiopoulos, MD, chief of our Vascular and Endovascular Surgery Division, and director of the Stony Brook Vascular Center, says:
"Stony Brook Medicine was the first New York State institution to participate in the Vascular Quality Initiative. In the past decade we have successfully utilized VQI data to improve patient care in our hospital. This second year in a row 3-star level designation is an acknowledgment of our focus on continuous improvement in the care of our patients."
Among his several leadership roles, Dr. Tassiopoulos is regional medical director of the Vascular Study Group of Greater New York (VSGGNY).
The VSGGNY functions under the auspices of the SVS Surgery Patient Safety Organization, and works cooperatively with other regional study groups, to benchmark outcomes after vascular procedures and assure that patients everywhere are receiving the highest quality of care possible.
Here at Stony Brook, Dr. Tassiopoulos is vice chair for quality and outcomes, and he has successfully directed several initiatives that ensure surgical quality and safety throughout the Department of Surgery.
Commenting on the achievement of our vascular team, Mark A. Talamini, MD, MBA, professor and chairman of surgery, and chief of surgical service at Stony Brook Medicine, says:
"This is a very big deal, when you think about the high-risk patient population and complex care that vascular patients require. To me this is an achievement on the level of our cardiac team's earning the highest quality rating of three stars from the Society of Thoracic Surgeons for their overall patient care and outcomes in isolated coronary artery bypass graft procedures."
Biannual regional VQI meetings allow physicians of different specialties, nurses, data managers, quality officers, and others to meet, share information and ideas, and learn from each other in a positive and supportive environment.
Members have used VQI data to significantly improve the delivery of vascular care at local, regional, and national levels, reducing complications and expenses.
"Hard-working, dedicated organizations such as Stony Brook Medicine are key to the success of the vascular registries," says VQI medical director Jens Eldrup-Jorgensen, MD.
"The work we do to build and maintain the registries for researcher use is crucial to health and outcomes for vascular patients. As the old saying says, 'if you can't measure it, you can't improve it.'"
Operating under the SVS, the VQI is composed of 12 registries containing demographic, clinical, procedural, and outcomes data from more than 500,000 vascular procedures performed nationwide and in Canada. The mission of VQI is to improve the quality, safety, effectiveness, and cost of vascular healthcare.
Posted by Stony Brook Surgery on July 5, 2019
Our Team Is First on Long Island to Use New Zenith Stent Graft

John Tanzi of Patchogue survived one of the most serious heart conditions a person can have — a catastrophic tear of his aorta.
He credits his recovery to the expertise of the Stony Brook Aortic Center, where he became the first person on Long Island to receive a new stent graft device that had just been approved for the treatment of aortic dissection.
The aorta is the main artery carrying oxygenated blood from the heart through the chest and abdomen. When it tears, the situation is a medical emergency.
The Stony Brook Aortic Center, led by Apostolos K. Tassiopoulos, MD, Thomas V. Bilfinger, MD, ScD, and Shang A. Loh, MD, is Suffolk County's only health resource that offers diagnosis and treatment for all aortic diseases.
Rapid Diagnosis and Treatment
On a recent winter morning, John was walking downstairs at his home in Patchogue when he stumbled and his right leg went numb. His wife Angela rushed him to Long Island Community Hospital, near their home. "They told my wife right away, 'We have to get him to Stony Brook if he's going to make it,'" John recalls. Stony Brook dispatched an ambulance for John and brought him to Stony Brook University Hospital under a "Code Aorta" protocol for rapid diagnosis and treatment.
Emergency Repair of John's Ascending Aorta
Henry J. Tannous, MD, chief of the Cardiothoracic Surgery Division and co-director of the Stony Brook Heart Institute, and Dr. Loh, vascular surgery residency program director and associate director of the Aortic Center, teamed up for the emergency repair of John's ascending aorta — the part of the aorta that immediately exits the heart and carries blood to the brain and arms — while keeping blood flow to the rest of his body.
"Basically, his aorta had split in half, and that's a dangerous situation," Dr. Tannous says. "When the first part of the aorta (exiting the heart) tears, the patient has a high risk of dying within hours."
John recalls now that when he woke up in the hospital, a week after being brought there with an aorta dissection, he met Dr. Tannous and Dr. Loh for the first time. "They're both good guys," he says. "They're very intelligent men and they know their jobs." After the surgery, "Everyone monitored me very carefully," John says.
The surgery was done in one of Stony Brook's hybrid operating rooms. These rooms, twice the size of a traditional operating room, have the usual surgical equipment plus sophisticated, real-time imaging systems mounted on a robotic arm that allow for precise guidance, allowing Stony Brook surgeons to perform complex procedures with greater safety and accuracy.
Preventing Future Risk
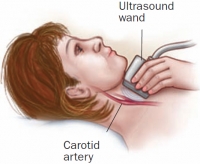
There would be more surgery to come. A follow-up CT scan revealed that parts of John's aorta in the chest and abdomen would put him at future risk for life-threatening complications because of the extent of the dissection, the shape of the tear and the size of his aorta. In preparation for the surgery to stabilize and heal John's aorta, Dr. Loh performed a type of bypass procedure, called a carotid-subclavian bypass, routing blood from one of the neck arteries to the left arm.
A New Stent-Graft System for Aortic Dissections
John's aorta dissection coincided with the release of a new stent-graft system designed specifically for aortic dissections. For the first time, using this stent, surgeons now can treat the entire aorta after a dissection instead of just the upper portion as they did previously.

"Before this device was approved, we only had stent-grafts that were originally designed to treat aneurysms – blood-filled bulges that result from weakening in a blood vessel's wall," says Dr. Loh. "We co-opted those stents into treatment for dissection, but the treatment was not ideal because we couldn't treat the lower portions of the aorta as a consequence of the numerous branch vessels present."
With the new device, the stent can be extended all the way down into areas that previously couldn't be treated.
"Now we're able to more completely treat the entire aorta after a dissection," Dr. Loh says.
"This allows us to prevent post-dissection complications, which include stroke, paralysis, aneurysm and even death."
Dr. Loh extended the stent to the point of John's aorta where it splits to each leg. After the minimally-invasive endovascular surgery, John was discharged home in a few days, while the open surgical repair would have kept him in the hospital for two to three weeks.
Recovering Well and Looking Forward
Today John is recovering well from that surgery. He has some back and shoulder pain, and walks with a cane, but he is steadily improving every day. He is looking forward to more good times with his family, including his daughter Valerie and his three-year-old grandson Anthony, and attending the wedding of his son Michael, in the fall.
"There's no way I want to miss this wedding," he says. At age 61, John's got a lot to look forward to.
John says he is grateful to his Stony Brook team. "I really have to compliment Stony Brook," he says. "It's like they gave me a reboot or reset. They got me going, and I feel pretty good — everybody did a wonderful job."
What Makes the Stony Brook Aortic Center Different
Our Aortic Center consists of a multidisciplinary team of specialists from cardiac imaging, cardiovascular medicine, anesthesiology, cardiothoracic surgery, and vascular surgery.
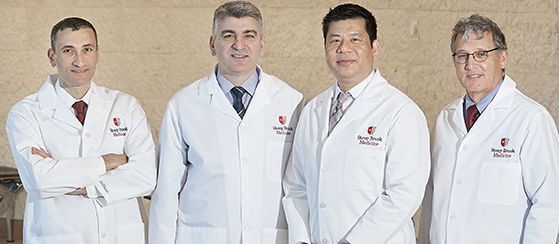
Leaders of the Aortic Center: (l to r) Dr. Henry J. Tannous, co-director, Stony Brook University Heart Institute, and chief, Cardiothoracic Surgery Division; Dr. Apostolos K. Tassiopoulos, chief, Vascular and Endovascular Surgery Division, director, Stony Brook Vascular Center, and co-director, Stony Brook Aortic Center; Dr. Shang A. Loh, associate director, Stony Brook Aortic Center; and Dr. Thomas V. Bilfinger, director, Thoracic Surgery Program, and co-director, Stony Brook Aortic Center.
"We collaborate with each other, and with the patient's referring physician, to find the most focused and cutting-edge solution to a patient's aortic disease," says Dr. Tassiopoulos.
"And patients don't have to travel far to receive advanced detection and treatment — the Stony Brook Aortic Center is Suffolk County's only facility offering patients comprehensive and coordinated care for the full range of aortic conditions."
| Acute aortic dissection is an infrequent but catastrophic disorder. Classically described as a patient complaining of an abrupt onset of severe "tearing" chest pain, presentations can often be more subtle. Until the advent of minimally invasive options for treating aortic dissections, medical management often failed, leading to aneurysm formation. Traditional open surgery for emergent complications of the dissection carried a high mortality and complication rate. With significantly lower mortality and complication rates, endovascular treatment of aortic dissections with stent grafts has become of the treatment of choice. |
Posted by Stony Brook Surgery on July 2, 2019
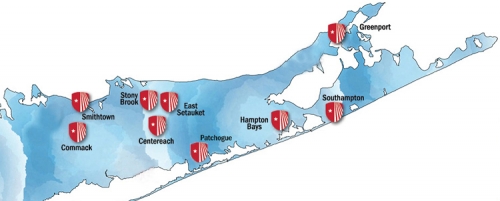
Eastern Long Island Hospital Joins Stony Brook Medicine Healthcare System
Today, Eastern Long Island Hospital (ELIH) became officially part of Stony Brook Medicine as the result of efforts toward this union over the past several years.
Located in Greenport at the eastern end of the North Fork, the acute care hospital will now be called Stony Brook Eastern Long Island Hospital (SBELIH).
This new name reflects combining the best in academic medicine and community medicine to improve access to advanced medical care for residents of the North Fork and Shelter Island.
The hospital was established in 1905, and has a long, distinguished history of serving its community, plus the vast number of people who go to the East End for their vacations in the summer months. It was the first hospital in all of Suffolk County, and the second on Long Island.
SBELIH has been formally affiliated with Stony Brook Medicine since 2006, with the decision for it to join the Stony Brook Medicine health system coming in 2015.
One of the principal goals now is for SBELIH to work collaboratively with Stony Brook University Hospital and Stony Brook Southampton Hospital to increase care, particularly specialized outpatient services.
New signage now identifies ELIH as Stony Brook Eastern Long Island Hospital
as its union with Stony Brook Medicine has been finalized.
These three hospitals in the Stony Brook Medicine healthcare system are working together to address healthcare gaps for East End residents, including specialty areas such as trauma, neurology, psychiatry, gynecology, pulmonology, hematology/oncology, and orthopedic services.
Stony Brook Medicine has maintained a fleet of critical care ambulances and first responders as a collaboration with community EMS and SBELIH to enhance the emergency care and transport services available to North Fork and Shelter Island residents.
Patients at SBELIH that require intensive care are transferred to University Hospital. As a result, patients quickly and easily receive treatment and benefit from enhanced services including shared medical records, clinical care protocols, and quality assurance programs.
"By welcoming Eastern Long Island Hospital into the Stony Brook Medicine Hospital System, we remain on the cutting edge of healthcare, implementing new strategies to improve the health of the communities we serve," says Kenneth Kaushansky, MD, MACP, senior vice president of Health Sciences and dean of the School of Medicine.
"We've taken many bold steps to strengthen our infrastructure across systems to promote excellence in research, education, and clinical services."
Our new Mastery in General Surgery Fellowship program is but one example of these steps. It provides Stony Brook surgical fellows with four months of rural surgery experience, thereby also improving surgical physician staffing in the SBELIH operating rooms and emergency department.
Paul Connor III, chief administrative officer of SBELIH, describes the new union with Stony Brook Medicine as "a marriage after a long courtship that links the two hospitals as the best way to serve the East End."
"With the help of Stony Brook Medicine," he says, "ELIH has gradually grown its footprint during the past few years."
SBELIH currently provides a range of surgical care including general surgery, colorectal surgery, neurosurgery, ophthalmology, orthopedics, plastic surgery, and urology.
With the new union the surgical services there will continue to grow and expand with increased on-site coverage by surgeons of Stony Brook Medicine. Plus, patients will have access to our surgeons and other providers at Stony Brook and in Southampton.
The general surgery team at SBELIH provides emergency general surgery care addressing trauma, appendicitis, bowel perforation, bowel obstruction, and gallbladder emergencies.
They have a practice of avoiding any prolonged hospitalization and, generally, their patients go from emergency room to the operating room to recovery to home the same day.
The general surgeons work with a top-notch anesthesia and nursing team to provide safe, continuous monitoring throughout the patient's hospitalization. They work closely with the outstanding physicians of the community to provide seamless care.
In general, along with their emergency room staff, they have the capability to handle any surgical emergency and stabilize the patient.
In the few cases where after stabilization the patient's condition mandates a higher level of care, they have a well-organized system in place.
Stony Brook Medicine, in conjunction with the Aviation Unit of the Suffolk County Police Department, will transfer patients to University Hospital.
SBELIH's surgeons have worked closely with Stony Brook Medicine for many years
to provide the highest level of surgical care for local patients.
SBELIH 's surgeons have worked closely with Stony Brook Medicine for many years to provide the highest level of surgical care for local patients.
In fact, they will only operate at SBELIH on elective patients when they feel the outcomes will be the best. This covers most cases including hernia, gallbladder, colon and rectal, stomach, and soft tissue.
They do the vast majority of our cases via minimally invasive techniques, primarily laparoscopy. They can provide the initial evaluation for patients with liver, pancreas, and other malignancies.
They then help coordinate the care in an interdisciplinary approach with oncology colleagues affiliated with SBELIH, often performing the biopsy and then coordinating the appropriate imaging studies.
This approach avoids delay to treatment. Patients are then offered access to our world-class oncologic surgeons at University Hospital. Time from initial visit to diagnosis and referral to a cancer specialist is generally less than two weeks.
Our relationship with Eastern Long Island Hospital is a longstanding one with a history of the two hospitals working closely together to improve healthcare access and quality.
Stony Brook Medicine clinicians have staffed and assisted in the development of SBELIH inpatient behavioral health programs, cared for patients who needed specialty services not available at SBELIH, and provided support and patient transport services during times of emergency.
For example, following damage from Hurricane Sandy, Eastern Long Island patients were transferred to University Hospital for care until the Greenport facility was restored.
The new union will allow SBELIH to work even more closely together with University Hospital and Southampton Hospital to improve healthcare quality and access, coordinate care, and improve efficiency for their patients through shared resources.
This will help ensure that the residents of the North Fork and beyond have continued access to high-quality coordinated care close to home — making sure that each patient receives the right level of care in the facility that is most appropriate to match the level of services needed.
In addition, the platform for academic training and research will be enhanced for both institutions across the spectrum of the health science centers.
There will be many surgical and other specialists arriving at SBELIH, based on demand, as a practice site is developed there for these doctors, and more services within the Stony Brook Medicine healthcare system are accessed.
| Stony Brook Eastern Long Island Hospital (SBELIH) is a 90-bed, full-service, community hospital committed to delivering excellence in patient care and meeting all the health needs of the North Fork and Shelter Island. Now a campus of Stony Brook University Hospital, SBELIH provides regional behavioral health programs serving the greater Suffolk County area. Centers of excellence include medical-surgical, advanced ambulatory care, behavioral health, emergency, geriatric, diagnostic services, physical therapy, and gastrointestinal services. Learn more about SBELIH. |
Posted by Stony Brook Surgery on June 26, 2019
Pregnancy or obesity stretches the skin over time. And as we age, the skin loses its ability to spring back into place after pregnancy or weight loss.
This lack of elasticity in the skin can cause extra skin folds of tissue — and an unflattering "love handle" around the belly and lower back.
Aging may also produce sagging skin and excess fat that impact the appearance of people in ways they might not find acceptable.
These physical changes may motivate people to seek procedures done by a plastic surgeon to regain natural shape and firmness.
There are two procedures popular today: tummy tuck (abdominoplasty) and lower body lift (belt lipectomy).
Here, Tara L. Huston, MD, associate professor of surgery and dermatology and a member of our Plastic and Reconstructive Surgery Division, answers frequently asked questions about tummy tuck and lower body lift.
Q: What is a tummy tuck?
A: A tummy tuck, also known as an abdominoplasty, is a term used to describe rejuvenation of the abdomen. The goal is to address some of the common physical changes that can occur following weight gain/loss as well as pregnancy.
Q: What cosmetic concerns can be treated with a tummy tuck?
A: Removal of excess skin and stress marks. Bulges above or below the belly button can be tightened to create a flat contour.
Q: How long after a tummy tuck are the desired results noticeable?
A: The swelling takes a few weeks to mostly resolve and a few months to completely resolve. However, the improved contour and skin quality may be seen immediately.
Q: What does the procedure entail?
A: First, the abdominal muscles are tightened to strengthen the midsection, decrease any bulging and narrow the waist. Second, the excess lower abdominal skin with stretch marks is removed.
Our plastic surgeons are true leaders in the field of plastic surgery: they not only provide cosmetic and reconstructive services but advance the art of plastic surgery
Q: Can a tummy tuck be combined with another procedure?
A: Yes, we will commonly work with gynecologists to pair with a uterine or ovarian procedure that requires an incision on the abdominal wall. We also frequently work with general surgeons when a hernia repair is done.
This team approach allows the patient to undergo one operation, one anesthetic, and one recovery while having two procedures.
Q: What is the difference between a full and mini tummy tuck?
A: In a full tummy tuck, both the upper and lower abdomen are addressed. This requires an incision along the lower abdomen from hip to hip as well as around the belly button. In a mini tummy tuck, primarily the lower abdomen is addressed. The lower abdominal scar is smaller, and there is no incision around the belly button.
Q: What is recovery from a tummy tuck like?
A: Patients generally go home the day of surgery and are encouraged to begin walking immediately. There are drains, but they will be removed by two weeks most of the time. We encourage our patients to plan four weeks of slow return to normal activities.
Q: What is the best time to resume exercise and sexual relations after the tummy tuck procedure?
A: In approximately four weeks.
Q: Is there much pain after surgery?
A: With muscle tightening, there is discomfort. However, we are able to manage this discomfort with muscle relaxants, non-narcotic medication such as acetaminophen, and narcotic medication when necessary.
Q: Is it okay to have tummy tuck surgery before having kids?
A: This is not recommended because the skin will stretch again and is unlikely to return to its tight postoperative state. It is better to wait if considering childbearing for the best long-term aesthetic result.
Q: What is a lower body lift?
A: A lower body lift is a tummy tuck that basically encircles the entire waist. This procedure is more common in massive weight loss patients.
Q: What cosmetic concerns can be treated with a lower body lift?
A: It helps to lift the gluteal (buttocks) regions as well as the lateral thighs.
Q: How long after a lower body lift are the desired results noticeable?
A: Similar to a tummy tuck, the swelling takes a few weeks to mostly resolve and a few months to completely resolve. However, the improved contour and skin quality on the abdomen, thighs, and buttocks may be appreciated immediately.
Q: What does the procedure entail?
A: A lower body lift is more involved than a tummy tuck because it requires surgery to be done on the back and then the front. First, the excess skin and tissue are removed from the back, and the incision is closed.
Next, the patient is turned over while still under anesthesia. The abdominal muscles are tightened to strengthen the midsection, decrease any bulging, and narrow the waist.
Lastly, the excess lower abdominal skin with stretch marks is removed from the front and joins the incision from the back.
Q: What is recovery from a lower body lift like?
A: Similar to a tummy tuck, you are encouraged to begin walking immediately. There are drains, but they will be removed by two to three weeks most of the time. We encourage you to plan four to six weeks of slow return to your normal activities.
Q: Is there much pain after surgery?
A: With muscle tightening and an incision that goes around the entire body, there is discomfort. However, we are able to manage this with muscle relaxants, non-narcotic medication such as acetaminophen and narcotic medication.
What our faculty have discovered allows them to incorporate the most novel surgical techniques with a safe surgical environment to provide our patients with the best surgical outcomes.
Q: Is it okay to have a lower body lift before having kids?
A: If there are chronic or hard to control rashes, open wounds, and sores that need to be addressed, this procedure is not recommended.
With pregnancy, the skin will stretch again, and is unlikely to return to its tight postoperative state. It is better to wait if considering childbearing for the best long-term aesthetic result.
Q: When is it advised to have both a tummy tuck and lower body lift?
A: It is more often recommended for patients who have undergone massive weight loss and who have enough excess skin around the posterior aspect of the body.
Q: What is the advantage of having tummy tuck and lower body lift done at Stony Brook Medicine?
A: First, we have plastic surgeons who are board certified in plastic surgery. This certification is relevant because many physicians who are not trained in plastic surgery are now doing "cosmetic" surgery.
Physicians not board certified in plastic surgery have not received the approved education, nor have they completed an examination process designed to assess the knowledge, experience, and skills required to provide high-quality plastic surgery.
Patients may put themselves at greater risk when using these non-certified physicians, many of whom are not even surgeons. The results of their work may be disappointing, even disfiguring, or lethal.
Another distinguishing factor about the care we provide is that our plastic surgeons are true leaders in the field of plastic surgery. They not only provide cosmetic and reconstructive services but advance the art of plastic surgery.
Some of the research done in our division focuses on patient safety and surgical outcomes. What our faculty have discovered allows them to incorporate the most novel surgical techniques with a safe surgical environment in order to provide our patients with the best surgical outcomes.
Finally, our plastic surgeons who specialize in tummy tuck and lower body lift have years of experience doing these procedures. Experience counts a lot, and so do the wonderful results that have made our patients happy they came to Stony Brook Medicine.
Posted by Stony Brook Surgery on June 21, 2019

Today is the first day of summer! For many, the summer months — when school is out and families take vacations — mean lots of fun in the sun. But with all the pleasures of the season come injuries and increased visits to the emergency room.
"During the summer, we treat more patients with injuries from burns, drownings, boating accidents, and motor vehicle crashes, than at any other time of the year," says James A. Vosswinkel, MD, chief of our Trauma, Emergency Surgery, and Surgical Critical Care Division, and medical director of Stony Brook Trauma Center.
"We want Long Islanders to get out and enjoy the warm summer months, but to take a moment to first think about safety and precautionary measures they can take when planning outdoor activities. Many of the accidents and deaths that we see are avoidable."
Watch Fireworks from a Distance, Don't Set Off at Home, and Practice Outdoor Fire Safety Tips: Nearly 10,000 Americans are injured by fireworks each year, according to the National Council of Fireworks Safety. Most of these injuries occur during the Fourth of July holiday and include serious burns, loss of fingers, and blindness.
"Each year, we treat adults and children injured by fireworks," says Steven Sandoval, MD, director of the Suffolk County Volunteer Firefighters Burn Center at Stony Brook Medicine. He recommends enjoying public firework displays, which are handled by professionals, from a safe distance — rather than setting them off at home.

Watch this PSA video (2:27 min) on the dangers of consumer fireworks.
And summertime burns also result from outdoor grills, both charcoal and propane, which cause hundreds of injuries and thousands of fires every year. "In addition, we treat at least a few injuries from fire pits and campfires every summer," says Dr. Sandoval. Fire safety tips include:
- Limit the amount of charcoal lighter fluid you use to start your fire pits and barbecues. A little goes a long way. And never pour any flammable liquid on hot coals or a live flame.
- Only use charcoal lighter fluids that are approved for cooking purposes.
- Keep children far away from fires and barbecue areas.
- Keep a bucket of sand and/or a garden hose nearby fire pits and barbeques in case the fire grows out of hand.
- Place the fire pit away from trees, branches, and foliage in order to prevent catching fire.
- Be sure your barbecue grill is well maintained and cleaned regularly.
- If you empty hot coals from your grill or fire pit, make sure they're not left anywhere where people can step on them. Even if you smother them with dirt or sand, if they're close to the surface someone could get a bad burn.
Dr. Sandoval emphasizes that flammable liquids, like wick (Zippo) lighter fluid, kerosene, and gasoline, should never be used to start a fire. "Unfortunately, the Burn Center treats flash burns to the face and torso when these agents have been used," Dr. Sandoval advises.
Closely Supervise Children around Fires: Around outdoor fires, Dr. Sandoval advises that children should be far enough away to prevent a burn injury. Remember to keep all barbecue accessories, including charcoal, lighter fluid, and propane gas tanks, well out of the reach of kids.

Keep a Watchful Eye on Swimming Children: Drowning is the leading cause of unintentional injury and death for children ages one to four, and drowning can occur in as little as two inches of water. "Parents should know that children can drown without making a sound, and that drowning deaths can occur even when children are left unattended for just a few minutes," says Dr. Vosswinkel.
Kristi L. Ladowski, MPH, injury prevention and outreach coordinator on our trauma team, provides the following water safety tips for people of all ages:
Tips to Keep Young Children Safe during Water Activities:
- It's all about supervision: always know where your children are, and never leave them alone near water, not even for a second:
- Designate a "water watcher" when children are swimming. The "water watcher" should not engage in any social distractions (conversation, phones, reading, etc.), they should only be watching the children in the pool for a set amount of time. Rotate the "water watcher" position so that the supervision remains fresh.
- Install physical barriers to keep children out of pool/spa areas: fences that children cannot climb with self-latching doors.
- Install door and/or pool alarms to notify you if a child is in or near the pool/spa.
- Do not use flotation devices (water wing, floaties) as a substitute for supervision.
- An adult should always be within arm's reach of infants and toddlers when they are in or around water:
- If a child goes missing, check the water first.
- Keep pools and spas covered when not in use, empty all other containers of water after use (buckets, inflatable pools).
- Remove all toys from in and around the pool when not in use.
Water Safety Tips for Adults and Older Children:
- Never swim alone, use the buddy system.
- If swimming in open bodies of water (oceans and lakes), only swim in designated areas and obey all instructions and orders from lifeguards.
- Do not dive into open bodies of water.
- Never swim under the influence of drugs or alcohol.
- Know how to safely get out of rip currents. If you're caught in a rip current:
- Stay calm.
- Don't fight the current.
- Escape the current by swimming in a direction following the shoreline (parallel to shore). When free of the current, swim at an angle — away from the current — toward shore.
- If you are unable to escape by swimming, float or tread water. When the current weakens, swim at an angle away from the current toward shore.
- If at any time you feel you will be unable to reach shore, draw attention to yourself: face the shore, call or wave for help.
Water Safety Tips for Everyone:
- Learn to swim.
- Learn CPR.
- Keep a cell phone nearby to call for help if needed.
- Take a water safety and rescue course.
- Keep rescue equipment nearby (life-saver ring, shepherd's hook).
- Wear a life jacket when boating. In 2016, 80% of boating deaths were caused by drowning and 83% of those who drowned were not wearing a life jacket. (For more on boating safety, download the U.S. Coast Guard's Boating Safety Guide.)
Alcohol and Water Don't Mix: According to the U.S. Coast Guard and the National Association of State Boating Law Administrators, alcohol can impair judgment, balance, vision, and reaction time. It can also increase fatigue and susceptibility to the effects of cold-water immersion. For boaters, intoxication can lead to slips on deck, falls overboard, or accidents at the dock.
"Alcohol impairs judgment and increases risk-taking, a dangerous combination for swimmers," says Dr. Vosswinkel. "Even experienced swimmers may venture farther than they should and not be able to return to shore, or they may not notice how chilled they're getting and develop hypothermia. Even around a pool, alcohol can have deadly consequences. Inebriated divers may collide with the diving board, or dive where the water is too shallow."
Summer Auto Safety Awareness Is No Surprise: We highly recommend the summer safety tips provided by the National Highway Traffic Safety Administration's (see here). They pertain not only to driving. One really important set addresses the risk of heatstroke when a child is left unattended in a parked vehicle. Remember:
- Never leave a child alone in a parked car, even with the windows rolled down, or air conditioning on. Children’s body temperature can heat up 3 to 5 times faster than adults.
- Always look in both the front and back of the vehicle before locking the door and walking away.
- Heatstroke can occur in temperatures as low as 57 degrees. On an 80-degree day, temperatures inside a vehicle can reach deadly levels in 10 minutes.
- Always lock your vehicle doors and trunk and keep the keys out of a child’s reach.
THE GOOD NEWS: MANY SUMMER ACCIDENTS ARE AVOIDABLE
"Overall, the good news is that many injuries that commonly occur during the summer are avoidable — or at least the risk of serious injury can be significantly reduced — if recommended safety precautions are taken," says Dr. Vosswinkel. "We encourage Long Islanders to keep safe and have a great summer!"
"But if an accident does occur, call 911 and go to the nearest emergency room," says Dr. Vosswinkel.
Posted by Stony Brook Surgery on June 11, 2019
Dupuytren's contracture (bent fingers) is a chronic condition that affects the hands and potentially cripples them. It's named after the French anatomist and military surgeon who popularized and first operated on it in the early nineteenth century, Guillaume Dupuytren (pronounced DOO-pwee-tren).
The underlying disease that causes the contracture in the hand is called Dupuytren's disease, which may or may not result in bent fingers. In other words, the disease does not always manifest itself as contracture. That said, it's a chronic progressive medical disease.
If everyone with any degree of Dupuytren's disease were counted, it's fairly common. In the United States alone, the number of Dupuytren sufferers projects to about ten million people, according to the Dupuytren Research Group.
While Dupuytren's contracture is more common among the elderly, the disease generally starts to appear in people in their forties to fifties, and increases in incidence after that. With increased life expectancy, Dupuytren's contracture has gained more medical and socioeconomic relevance.
The contracture can impact people in many ways — from writing to washing one's body, from picking up small things to playing musical instruments, shaking hands, caressing a loved one, and so forth — because our hands are so important in every part of our day.
In addition to well-known familial and genetic causes, other environmental factors such as nicotine, diabetes, alcohol, and trauma are associated with causing Dupuytren's disease and contracture.
Here, Alexander B. Dagum, MD, chief of our Plastic and Reconstructive Surgery Division, answers frequently asked questions about this condition. A distinguished expert, he is fellowship trained in hand surgery as well as plastic surgery, and board certified in both specialties.
Q: What is Dupuytren's disease?
A: Dupuytren's disease is a progressive condition that affects the tissue underneath the skin that is called the fascia. The fascia is responsible for holding the palm skin taught so it does not slide around when one grips or grasps an object. Tough scar is laid down on the fascia that gradually contracts, leading to bent fingers that cannot be straightened.
Stony Brook Medicine is considered one of the world's foremost institutions
when it comes to the treatment of Dupuytren's disease.
Q: What causes Dupuytren's disease?
A: The cause is unknown, but there is a genetic component. A positive family history, in particular, plays an important role in the development of Dupuytren's disease. Other factors known to make Dupuytren's disease worse are excessive alcohol consumption, diabetes, smoking, and epilepsy and certain antiepileptic medication
Q: How is Dupuytren's disease diagnosed?
A: Dupuytren's disease is diagnosed clinically by physical examination. It usually starts with a nodule in the palm underneath the skin that is firm and can initially be painful. There may be associated pits between the nodules that develop subsequent to this.
As the disease progresses, the nodules become cords underneath the palm and finger that start to contract and cause the fingers to bend.
Patients may also develop nodules over the dorsal knuckles known as the knuckle pads of Garrod or disease elsewhere, such as in the feet (Lederhose disease) or penis (Peyronie disease).
Q: Who gets Dupuytren's disease?
A: There is a genetic predilection to affect primarily people of Northern European or British descent. That is why it is also known as the Viking disease as it is felt it originated in people of Scandinavian ancestry and subsequently spread from there. However, it has been reported in all races. It affects men more often than woman, and usually starts after age 40.
Q: What happens if Dupuytren's disease goes untreated?
A: The fingers progressively bend and contract, leading to inability to open the hand and decreasing hand function.
Q: Is there a cure for Dupuytren's disease?
A: There is no cure for Dupuytren's disease, but it can be treated with surgery or injections to remove or dissolve, respectively, the cords causing disabling contractures.
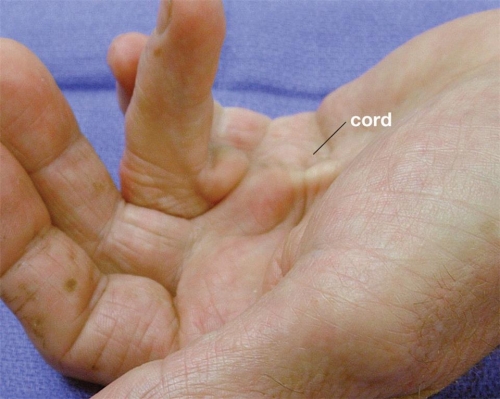
| Advanced case of Dupuytren's contracture showing cord leading to bending of the ring finger into the palm (click to enlarge). |
Q: What is Dupuytren's contracture?
A: When a hand cord caused by Dupuytren's disease leads to a bent finger that can no longer be fully extended, the condition is called Dupuytren's contracture.
Q: What are the risk factors for Dupuytren's contracture?
A: The risk factors for Dupuytren's contracture are the same as for the disease, but a strong family history, early onset of the disease (before age 40), disease in both right and left hand, associated disease in the knuckle pads, feet, or penis will increase the risk of developing contractures.
A history of diabetes, heavy alcohol consumption, smoking, and epilepsy and certain antiepileptic medications will also increase the risk of developing contractures.
Q: How does Dupuytren's contracture impact a person's life?
A: The inability to open the fingers fully may make it difficult to grip and grasp objects such as tools, instruments, a golf club, and so forth. The fingers also may get jammed and injured easily as the person reaches out to grab an object or puts their hand in their pocket.
Q: Can Dupuytren's contracture occur in any finger?
A: Yes, but it most commonly affects the ring finger followed by the small finger.
Q: How is Dupuytren's contracture treated?
A: Traditionally, Dupuytren's contracture is treated with surgery to remove the diseased fascia (tissue) and, thereby, correct the contracture.
Although the surgery is done on an outpatient basis, the recovery can be strenuous for some patients, and almost always requires a six-week course of hand therapy and splinting.
Recently, with the development of an enzyme (collagenase) known as Xiaflex, we can inject the cords in the office to dissolve the diseased cords, and subsequently 24 to 96 hours later manipulate the bent finger under local anesthesia, rupturing the cords and correcting the contracture.
Another method that has become popular is a minimally invasive surgical method known as needle aponeurotomy, where under local anesthesia a needle is used to break apart the cord.
Hand surgeons have come from all over the world to Stony Brook Medicine
to learn about Dupuytren's disease and its treatment.
Q: Which treatment for Dupuytren's contracture is better: surgical or non-surgical?
A: The early results for surgery versus enzyme injection have been equivalent. The long-term results are not yet available. The disease is not cured and, thus, recurrence or extension of the disease with the same or other contractures occurs in at least 20% of patients.
Q: What is the advantage of having Dupuytren's contracture treated at Stony Brook Medicine?
A: Stony Brook Medicine is considered one of the world's foremost institutions when it comes to the treatment of Dupuytren's disease.
The enzyme (collagenase) treatment known as Xiaflex used throughout the world to treat this disorder non-surgically was developed at Stony Brook.
Surgeons have come from all over the world to learn not only about Dupuytren's disease and its treatment, but also how to use Xiaflex to treat Dupuytren's contracture.
Several thousands of patients have been treated here with either surgery or enzyme injection, making Stony Brook Medicine not only the busiest but the most experienced center for Dupuytren's disease in the country.
Posted by Stony Brook Surgery on June 6, 2019
This year's Research Day program took place last Thursday at Stony Brook University's Charles B. Wang Center, and was another great success, as the event continues to grow, with more research presentations and increased attendance.
The morning forum showcased ongoing and completed research projects by way of oral platform presentations, as well as a poster competition by our residents, medical students, and faculty.
Opening the program, Kenneth Kaushansky, MD, MACP, dean of the School of Medicine and senior vice president of health sciences, said:
"I have attended virtually every Research Day since its inception, and I am very pleased to see the quality of research grow and the amount of research grow, together with the new horizons of research on display here today."
Dr. Kaushansky emphasized that Stony Brook Medicine is home to an abundance of leading-edge multidisciplinary research that's advancing healthcare not only in our region but around the world, from neuroscience to surgery and in numerous other disciplines.
Stony Brook Medicine is committed to making research happen, says Mark A. Talamini, MD, MBA, professor and chairman of surgery and chief of surgical services at Stony Brook Medicine.
Dr. Talamini opened his welcome remarks by saying Research Day is about "what we are all here to do — to advance patient care through research and discovery."
Our Research Day celebrates our discoveries, and also demonstrates that as academic surgeons our faculty not only has the job to take care of patients, but to make surgery better. This is what sets us apart from private-practice surgeons.
Research Day demonstrates how we're making surgery better and what sets us apart.
The program included 50 posters presenting study abstracts, plus five oral presentations moderated by faculty discussants, and it attracted over a hundred attendees from Stony Brook Medicine and the University community.
The keynote speaker was Ramin Parsey, MD, PhD, professor and chairman of psychiatry and behavioral health, and director of positron emission tomography (PET) research.
A leader in developing National Institutes of Health (NIH) and industry-sponsored imaging and clinical protocols, Dr. Parsey conducts research in advanced brain imaging data acquisition and analysis. He has had continuous NIH funding for more than a decade.
Dr. Parsey's brain imaging research systematically addresses the problem of treatment resistance, collaborating across disciplines to engage investigators at the boundary of physical and medical sciences to identify biomarkers to predict treatment response.
Among his research achievements, Dr. Parsey has developed an advanced imaging method for the diagnosis of Alzheimer's disease, as well as novel radiotracers for PET imaging of the brain.
Dr. Parsey's address, titled "Lack of Reproducibility and Ending Medical Reversals and an Update on PET Imaging at SBU," was extremely thought-provoking.
Dr. Parsey addressed the issue of research findings that can't be reproduced by other researchers who attempt to reproduce them, and the need to end medical practices that show no benefit to patients. He presented data showing numerous attempts to reproduce published studies that failed.
He argued that aggressive critical thinking in the analysis of data is needed to determine its real value. Correlations, he pointed out, may merely be coincidental and have no causal relationship. He referenced the lampoon "dead salmon study" to further his argument.
Commenting on the purpose of Research Day, A. Laurie W. Shroyer, PhD, MSHA, professor of surgery and vice chair for research, who oversees the event, says: "Research Day shows the commitment of our department to advancing scientific knowledge in order to improve patient care and population health.
"Residents, medical students, and fellows, as well as faculty, utilize their research projects to address important clinical questions that they face each day, fostering their curiosity and building their excitement and enthusiasm for current and future biomedical research.
"By networking at events such as Research Day, they gain new opportunities for collaborative multidisciplinary team projects. Most important, our Research Day lights the pathway for trainees to envision a future career in academics."
Research Day lights the pathway for trainees to envision a future career in academics.
All categorical residents in our general surgery residency program are required to conduct at least one research project each year, and to present their studies at the Research Day program.
All of our residency programs are committed to training physician-scientists who can both practice and advance surgery in their careers after they graduate from Stony Brook.
Established in 2010, Research Day is an opportunity for our residents as well as our faculty and medical students to present their surgical research. The focus of the program is moving the science of surgery forward.
The Research Day program offers continuing medical education (CME) credit; this activity is designated for a maximum of 3.0 AMA PRA Category 1 Credits™.
Here are the titles/authors of the posters exhibited at this year's Research Day. Together, they demonstrate the broad range of research activity within the Department of Surgery, and the impressive productivity of our residents and students:
- A case report of Guillain-Barre syndrome following thermal burn and subsequent Takotsobu cardiomyopathy | Diep G, Frost M, Jacquez R, Sandoval S.
- A comparison of the effects of negative pressure wound therapy (NPWT) and standard surgical dressings (SSD) on outcomes in wounds after resection of a malignancy: a systematic review | Singh G, Hays T, Shekar S, Marquez J, Khan F, Khan S, Dagum A, Bui D.
- A proposal for the evaluation of neurological, renal, and respiratory outcomes during extracorporeal life support, a QA initiative | Noubani M, Seifert F, McLarty A.
- A review of the diagnosis and management of male breast cancer | Wolchok C, Chow P, Kapenhas E.
- An iatrogenic biliary duct injury to a right posterior sectorial duct | Zohourlan, T, Allendorf J, Levine J.
- Anal and perianal Paget's Disease: reviewing the literature to create a case series and discover new insights | Basishvili G, Dickler C, Yelika S, Carey E, Fong C, Denoya P.
- Analysis of long-term outcomes of ventral hernia repair performed by plastic surgeons and general surgeons: a single institution review | Jou C, Perzia B, Mellia J, Carey E, Kapadia K, Sing G, Marquez J, Khan S.
- Analysis of NSQIP readmissions after general and vascular surgical intervention at a single institution: our experience | Jasinski P, Shah A, Tassiopoulous A. Oral Presentation.
- Analysis of robotic assisted sialolithotomy with sialoendoscopy for management of large submandibular stones | Chao E, Alrassi J, Samara G.
- Anastomotic ulcer continues to be a major source of morbidity over the time following gastric bypass | Pyke O, Yang J, cohn T, Yin D, Docimo S, Talamini M, Bates A, Pryor A, Spaniolas K.
- Association of inferior vena cava filter placement for patients with venous thromboembolism and a contraindication to anticoagulation with 30-day mortality | Patel R, Skripochnik E, Loh S.
- Avoiding the trap of misdiagnosis: valuable teaching points derived from a case of longstanding popliteal artery entrapment syndrome | Wady H, Badar Z, Farooq Z, Shaw P, Kobayashi K.
- Barriers to body contour surgery in post-bariatric patients: is cost the only factor? | Kapadia K, Marquez J, Huston T.
- Bedside ultrasound assessment of diaphragm function in traumatic rib fractures: an update | O'Hara D, Randazzo S, Ahmad S, Pasternak D, Huang E, Jawa R.
- Cancer recurrence and the use of a vacuum assisted closure therapy in a rat model | Kaymakcalan O, Singh G, Uddin Z, Abbas A, Hays T, Bui D, Khan S, Khan F, Dagum A.
- Characterization of differences between arterial and venous thrombosis | Singh G, Chuang YC, Joshi I, Lee S, Bannazadeh M, Sikalas N, Labropoulos N.
- Chronic femoral artery pseudoaneurysm with associated high output arteriovenous fistula | Harrington A, Kokkosis A, Labropoulos N.
- Comparison of males and females presenting for peripheral vascular intervention of superficial femoral artery and popliteal artery in the national VQI database | Jasinski P, Yun J, Labropoulos N, Kim H, Kokkosis A.
- Demographics and outcomes of the acutely intoxicated patient | Fleury M, Ng C, Hakmi H, Jawa R. Oral Presentation.
- Development of pneumomediastinum after transcarotid artery revascularization (TCAR).
- Case report and literature review | Drakos P, Terrana L.
- Do national databases underestimate complications in ventral hernia repair? A single institution's perspective | Perzia B, Jou C, Mellia J, Carey E, Kapadia B, Singh G, Marquez J, Khan S.
- Does an educational module on the function and use of nasogastric tubes improve nursing compliance with their management? | Ferrara A, Jasinski P, Wertheim W, Kantor L.
- Emergent versus elective ostomies for colon cancer: is there a difference? | Thompson H, Altieri M, Yang J, Sun S, Genua J, Pryor A. Finalist in Outstanding Poster Competition.
- Endotunnel: a novel surgical wound protector | Hsi H, Talamini M.
- Evaluation of long-term complications and recurrence rates in ventral hernia repair with component separation | Jou C, Mellia J, Perzia B, Carey E, Kapadia K, Singh G, Marquez J, Khan S.
- Extra-anatomic aortic bypass via an ascending aorta-descending aorta retrocardiac tunnel during excision of an infected TEVAR graft | Rabenstein A, Bilfinger T, McLarty A.
- Incidence of appendectomy after abdominal wall reconstruction | Simon J, Docimo S, Spaniolas K.
- Institutional review of stereotactic body radiotherapy (SBRT) with curative-intent chemoradiation in patients with oligometastatic non-small cell lung cancer (NSCLC) | Tembelis M, Alam W, Grossman C.
- Is the glass-ceiling higher than we think? Gender disparity trends in physician executive positions and academic plastic surgery | Marquez J, Zaransky S, Ikizoglu M, Singh G, Huston T.
- Isolated extra-axillary lymph nodes in a case of invasive ductal carcinoma of the breast: case report and literature review | Wolchok C, Zorn J, Kapenhas E.

- Isolating hip fractures: admission to trauma service improves outcomes | Rubano J, Jacquez R, Paccione M, Shapiro M, McCormack J, Huang E, Vosswinkel J, Jawa R. Finalist in Outstanding Poster Competition.
- Large non-infectious granulomatous adenitis in children needs surgical excision for cure | Obeid J, Bongu S, Burjonrappa S.
- Management of gastric perforations using natural orifice transluminal endoscopic surgery | Basishvili G.
- Majority of patients undergoing colorectal cancer resection 2010-2018 have not participated in colorectal screening programs | Fong C, Joseph DF, Munaganuru N, Channer B, LaComb JF, Li E, Denoya P. Winner of Outstanding Poster Competition.
- Mid-term outcomes of thrombolysis for acute lower extremity ischemia at a tertiary care center | Skripochnik E, Bannazadeh M, Jasinski P, Loh S. Finalist in Outstanding Poster Competition.
- Natural history of isolated distal deep vein thromboses | Hirai K, Labropoulos N.
- Outcome of open inferior vena cava reconstruction | Tzavellas G, Bannazadeh M, Sikalas N, Landau D, Loh S, Bilfinger T, Tassiopoulos A.
- Parathyroid hormone level alone is the most accurate predictor of intravenous calcium administration after thyroidectomy | Masson R.
- Percutaneous endoscopic gastrostomy replacement with laparoscopic assistance: a case report | Laskowski R, Karim S, Jasinski P, Sbayi S.
- Postoperative Prophylactic antibiotics is not necessary in tissue-expander breast reconstruction: a single-institution's change in protocol | Marquez J, Ghosh K, Kapadia K, Ferrier A, Medrano C, Marmor W, Singh G, Vasilakis V, Huston T, Ganz J, Khan S, Dagum A, Bui D.
- Prevalence of Delayed Intracranial Hemorrhage in trauma patients on Novel anticoagulant and/or antiplatelet therapy | Lacey R, Jawa R.
- Primary use of endoanchors in patients with hostile aortic neck anatomy offers protection from proximal seal zone complications | Ribner A, Sandowski S, Tzavellas G, Kokkosis A, Tassiopoulos A.
- Propensity matched comparison of band to Roux-en-Y gastric bypass (BtoRYGB ) vs primary Roux-en-Y gastric bypass (PRYGB) | Robins F, Tatarian T, Spaniolas K.
- The psychiatric impact of medical and other trauma on adult urological procedures | Chen A, Xu Y, Egan J, Feustel P, De E. Finalist in Outstanding Poster Competition.
- Quantifying ambulation after routine bariatric surgery to predict post-operative hospital stay and complication rates | Weller R.
- Radiographic assessment of abdominal wall musculature post-bariatric surgery | Malino C, Docimo S.
- Retrospective evaluation of trauma team activations made via SBUH HEMS | Maloney L, Chan R.
- Role of leupeptin in preventing hind limb ischemic tissue injury | Singh G, Gurevich M, Martin I, Khan S, Bui D, Komatsu D, Dagum A. Oral Presentation.
- Safety of Bariatric Surgery in patients older than 65 | Goldberg I, Cohn T, Docimo S, Bates A, Spaniolas K, Pryor A. Oral Presentation.
- Seimens Artis Pheno System significantly reduces radiation delivery compared to older models during lower extremity procedures | Cheung E, Skripochnik E, Loh S.
- Socioeconomic and gender disparities in anal cancer diagnosis and treatment | Celie KB, Jackson C, Agrawal S, Dodhia C, Guzman C, Kaufman T, Hellenthal N, Monie D, Monzon J, Oceguera L.
- Systematic review on the prevalence of venous thromboembolism and bleeding in abdominoplasty patients | Perzia B, Marquez J, Vasilakis V, Labropoulos N, Khan S.
- Temporal and spatial profile of fibrin within the mice model of deep vein thrombosis | Singh G, Chuang YC, Joshi I, Lee S, Bannazadeh M, Sikalas N, Labropoulos N.
- The association between adoption of an acute care surgery service model and volume of laparoscopic cholecystectomy at a tertiary care center | Yelika S, Kirschen G, Sbayi S, Pryor A.
- The safety and efficacy of utilizing negative pressure wound therapy after sarcoma resection | Restle D, Klein G, Khan F, Khan S, Ganz J, Bui D.
- Umbilicoplasty techniques: a comparative study of aesthetic outcomes | Nasser A, Brewer B, Douglas B, Reish R, Glickman L.
- Using relational coordination survey tool to quantify relationships necessary for catheter care | Sreeramoju P, Connally R, Thompson H, Altieri M, Yang J, Sun S, Genua J, Pryor A.
- VA-ECMO outcomes in a single institution; role of diagnosis, age, BMI, and on-going CPR | Rabenstein A, Chiu R, Seifert F, McLarty A.
- Validation of benchmarks for an upper gastrointestinal endoscopy simulation trainer for use in residency training | Park J.
- Venous thromboembolism versus bleeding events in massive weight loss patients undergoing single body contouring procedures: a systematic review and pooled analysis | Yin C, Marquez J, McAuliffe P, Vasilakis V, Estralla J, Labropoulos.
Posted by Stony Brook Surgery on June 4, 2019
Advancing the Care of Women with Pelvic Venous Disorder
Chronic pelvic pain (CPP) is very common in women and can potentially lead to significant disability. Approximately one out of every three women will suffer from pelvic pain at some point during their lifetime.
CPP is defined as pain that occurs in the pelvic area (below the belly button) and lasts for at least six months. It may or may not be associated with menstrual periods.
One of the possible causes of CPP is the presence of varicose veins around the ovaries and uterus. In normal pelvic veins, blood flows through the ovarian veins toward the heart. The ovarian veins, like veins throughout the body, have one-way valves that prevent blood from flowing backwards.
When the ovarian veins dilate (stretch beyond normal dimensions), the valves do not close properly, resulting in backward flow of blood, also known as reflux. Consequently, there is pooling of blood within the pelvis that may lead to pelvic varicose veins and pain.
This condition along with the presence of relevant symptoms has been known as pelvic congestion syndrome (PCS).
Symptoms of PCS may include non-cyclic pain, heaviness, bloating or aching in the pelvic area which worsens with prolonged standing and can be relieved with lying down.
Pelvic varicose veins as a possible cause of chronic pelvic pain tend not to loom large for most physicians, so an evaluation by a vein specialist with expertise in pelvic vein disease is needed for proper care.
Some patients may experience worsening of symptoms during their menstrual cycle or after sexual activity. They may also experience frequency of or pain during urination.
The fact that these symptoms can have a range of causes and that pelvic varicose veins tend not to loom large for most physicians necessitates an evaluation by a vein specialist with expertise in pelvic vein disease.
The cause of PCS is unclear. However, the possibility of anatomic or hormonal abnormalities or dysfunction can contribute to its development. Most of the affected women are between the ages of 20 and 45 years, and have a history of two or more pregnancies.
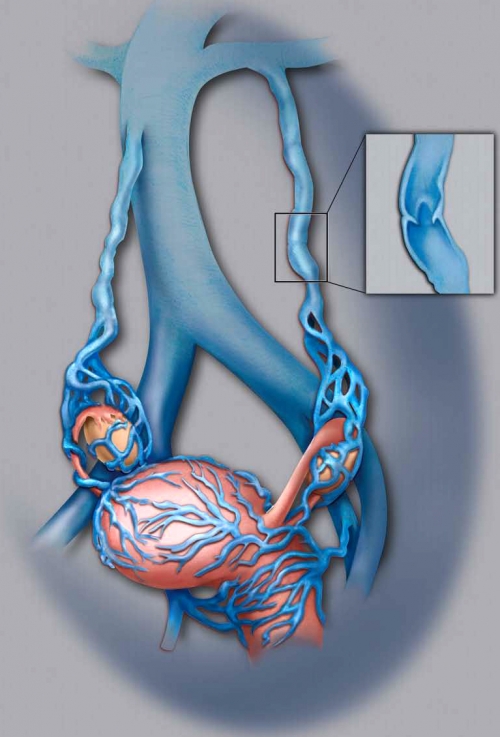
| Dilated ovarian veins with abnormal valves leading to reflux and development of varicose veins around the ovaries and uterus (note close-up of varicose vein). Click on image to enlarge. |
The good news is, there is a minimally invasive non-surgical way to treat PCS (read more). The bad news is, PCS remains poorly understood by the vast majority of physicians. As a result, women with PCS too often do not receive the care they need and the pain relief they seek. But, recently, there have been increased efforts to improve awareness of this clinical condition.
Historically, the different venous causes of pelvic varicose veins have been independently described as an unrelated group of "syndromes" (pelvic congestion, May-Thurner, nutcracker) that refer to specific anatomic aberrations but fail to completely account for the underlying vein-related causes and overlapping spectrum of symptoms and signs.
For this reason, PCS has recently been renamed pelvic venous disorder (PeVD) which incorporates all the potential different causes of pelvic varicose veins.
Although there has been increased PeVD awareness in recent years by vascular/vein specialists, it continues to be underdiagnosed and undertreated, even by OB-GYN specialists.
In a recent study, 8% of premenopausal women with CPP of unclear causes were found to have dilated pelvic veins on CT scan, which could have explained the reason for their CPP.
The good news is that increased efforts are now underway to improve awareness of PeVD, and Stony Brook Medicine is an active member of the progress team to advance care for women.
To advance the care of women with PeVD, a multidisciplinary pelvic work group has initiated several projects to increase knowledge about it. This group includes vascular surgeons, interventional radiologists and vein specialists.
The pelvic work group is collaborating with multiple medical societies and organizations around the world — some of which are the American Vein and Lymphatic Society, American Venous Forum, Society of Interventional Radiology, European Venous Forum, International Union of Phlebology, American College of Obstetricians and Gynecologists, and International Pelvic Pain Society — which are endorsing and supporting these projects.
Stony Brook Medicine has developed a diagnostic protocol to identify PeVD using non-invasive ultrasound, has published clinical work to enhance the understanding about PeVD and participates in several new projects in this field.
The first task of the pelvic work group was to develop a classification system for PeVD. A PeVD treatment descriptive tool is also being developed to help define an effective treatment strategy based on the classification system as it relates to the type and location of disease.
The next step was to create a quality-of-life questionnaire that is specific for PeVD, and to validate this tool. This project is in its early phases. A protocol for a multicenter randomized study of the tool, plus the effect of treatment, is currently under design.
In March of 2019, a multidisciplinary panel assembled by the Society of Interventional Radiology published a paper presenting its recommendations for future research needed to close the multiple evidence gaps that existed related to PeVD. It also provided a good account of why physicians who are not vein specialists rarely consider the diagnosis.
Given the lack of broadly accepted methods to evaluate and diagnose women, the potential that some are being treated inappropriately with pelvic venous interventions is also concerning.
The panel recommended international multidisciplinary involvement in the research agenda with the goal of gaining broad endorsement of the disease definitions and tools.
The panel was clear that it is necessary to first develop the required research tools to ensure that the financial and time investments made to support PeVD research would yield evidence that will be broadly accepted.
Stony Brook's participation as members of the pelvic work group — based on our extensive experience in the diagnosis and treatment of PeVD — is part of the current effort to advance care for women with it.
The Stony Brook Center for Vein Care will continue to serve as a leader to provide women with a PeVD the most appropriate care to relieve their pelvic pain and help them to return to an active life.
| Pelvic venous disorders (PeVDs) in women can present with chronic pelvic pain, lower-extremity and vulvar varicosities, lower-extremity swelling and pain, and left-flank pain and hematuria. Multiple evidence gaps exist related to PeVDs with the consequence that nonvascular specialists rarely consider the diagnosis. Recognizing this, the Society of Interventional Radiology Foundation funded a Research Consensus Panel to prioritize a research agenda to address these gaps. — "Research Priorities in Pelvic Venous Disorders in Women," Journal of Vascular and Interventional Radiology (2019) |
Posted by Stony Brook Surgery on May 30, 2019
Read about How We Are Leading the Way in Patient Care, Education, and Research
| "The Stony Brook University Department of Surgery was founded in 1974 following the opening of the School of Medicine, in 1971, under the visionary leadership of Edmund D. Pellegrino, MD, the first dean of medicine and first vice president of health sciences at Stony Brook.… Mark A. Talamini, MD, joined the Department of Surgery as chairman in 2013, the fifth in our history. He is a national leader with a history of surgical innovation." — From "History of Our Department: 1974 to Present" |
Read POST-OP online now. To receive a complimentary free subscription to the print edition of POST-OP, please send request with your complete postal mailing address.
Posted by Stony Brook Surgery on May 28, 2019
Help Decrease the Number and Severity of ATV Accidents Involving Children
Summer is almost upon us and kids will be out of school! If your family enjoys riding all-terrain vehicles (ATVs), we want you to be safe. June 1-9 is ATV Safety Week, starting this Saturday.
Every year children are injured riding ATVs. The American Academy of Pediatrics strongly discourages children under the age of 16 from riding ATVs because of the serious potential harm.
Despite this, many children still ride ATVs; therefore, it is important to educate children and their parents on ATV safety.
ATV safety education can help decrease the number and severity of ATV accidents involving children.
What do we know about the dangers of the use of ATVs by children and youth?
The United States Consumer Product Safety Commission collects data and reports annually on ATV-related injuries. Here's what the 2016 report, issued last December, says:
New York State ranks within the top 10 states where people (adults and children) die from ATV-related accidents.
In New York State, more than six children are injured every day due to ATV-related accidents.
From 1982 through 2016, there were 3,232 ATV-related fatalities of children younger than 16 years of age, which accounts for 22% of total ATV-related deaths.
Children under the age of 16 lack the judgement and physical ability to safely drive ATVs,
according to the American Academy of Pediatrics and American Pediatric Surgical Association.
Of the 3,232 reported ATV-related fatalities of children less than 16 years of age, 44% (1,411) were younger than 12 years of age. This mortality is disproportionately high relative to the number of children riding ATVs.
Nearly one-third of children hospitalized after an accident on an ATV suffer a traumatic brain injury.
More than 90% of ATV-related injuries involving children can be attributed to a lack of developmental skills needed to maneuver the faster, more powerful adult ATVs. Children under 16 years lack the developmental skills to safely drive adult ATVs.
What are the New York State laws?
All ATVs must be registered with the Department of Motor Vehicles (DMV) if it is operated anywhere in New York State — including on an owner's property. Registration must be renewed yearly.
You may not operate any ATV anywhere in New York State, except on your own property, unless it is covered by liability insurance.
No passengers are allowed on the ATV unless it is designed to carry more than one person. "Single-rider" ATVs are intended for use by a single driver and no passenger. "Two-up" ATVs are designed for an operator and one passenger only.
All riders (operator and passengers) must at all times wear a helmet approved by the US Department of Transportation (USDOT). It is also recommended that you wear a face shield or goggles, protective clothes, and footwear.
ATV use on highways is prohibited, except to cross these roads. (Public highway means any highway, road, alley, street, avenue, public place, public driveway, or any other public way). ATV use is also prohibited on public land.
You do not need a driver's license to operate an ATV in New York State, but the following restrictions apply to children under age 16:
- Less than 10 years of age may ride an ATV only when under adult supervision, or without adult supervision only when on lands owned or leased by your parent or guardian.
- 10 to 15 years of age may ride an ATV if they are on their parent's land and supervised by a parent, or on their parent's land and in possession of a safety training certificate earned after completing an ATV safety training course approved by the DMV.
No ATV shall be operated without a lighted headlight and taillight from one half hour after sunset to one half hour before sunrise.
Both the owner and the operator of an ATV may be held liable for injury and/or damages resulting from an ATV accident.
What are some safety recommendations?
Erica R. Gross, MD, assistant professor of surgery in our Pediatric Surgery Division, says:
"The increasing popularity of ATV use with its associated risk of permanent injury underscores the need for increased safety awareness among the general public.
"With summer on the horizon, now is the time to act to help prevent ATV accidents. It must be emphasized that non-fatal ATV accidents can result in catastrophic, life-changing medical problems. We need to protect our children from them.
"That's why I think the Trauma Committee of the American Pediatric Surgical Association offers an especially good set of recommendations for ATV use."
The safety recommendations of the American Pediatric Surgical Association Trauma Committee are:
1. The strongest recommendation is that children younger than 16 years lack the judgment and physical ability to safely operate motorized vehicles, and therefore should not operate ATVs of any size. However, the committee recognizes that many parents will find this recommendation unacceptable.
For those parents with children younger than 16 years who choose to allow their children to operate an ATV, the committee recommends that only ATVs designed for younger children (i.e., 900-cc engine or less) be operated, that no child less than 12 years be allowed to operate an ATV, and that these other recommendations be followed:
2. Children between ages 16 and 18 should ride age appropriate vehicles with an engine size no greater than 350 cc and should be supervised by a responsible adult. As mentioned above, children between ages 12 and 15 should only operate ATVs with engine sizes appropriate for smaller children, generally less than 90 cc.
3. ATV drivers should complete an approved and age-appropriate training course.
4. ATVs are designed for a single rider, and no passenger of any age should ever be on board. This includes the recommendation that children not ride as passengers on ATVs with adult drivers.
5. ATV operators should always wear a government approved helmet, eye protection and appropriate protective clothing.
6. ATVs are intended for off-road use and should not be used on public roads.
7. No one should drive an ATV while under the influence of alcohol or other substances that can impair judgment, insight, and reaction time.
8. ATVs should not be used after dark.
How do you know when your child is ready to ride an ATV?
The size of your child is not the only determinant. Children must have strength, skills, and good judgment to safely operate an ATV. Please review the ATV Safety Institute Readiness Checklist.
ATV Training Courses: The ATV RiderCourse is a half-day hands-on training program and is available nationwide. Please visit the website of the ATV Safety Institute, or call there at 800-887-2887 to find the program nearest to you.
ATVs are designed to be driven on off-road terrain, and are difficult to control on paved roads where they are at risk of overturning or colliding with cars and trucks.
| ATV-related injuries vary depending on incident characteristics and patient populations. On-road use incurs a significant increase in injury severity. The pediatric population is significantly more likely to incur a severe injury and the presenting injury pattern differs from the adult population. Knowledge of population and presentation trends can help direct trauma care providers in the care and management of injured ATV riders. — "Increasing Incidence of All-Terrain Vehicle Trauma Admissions in the Pediatric and Adult Populations," International Journal of Orthopaedic and Trauma Nursing (2018) |
Posted by Stony Brook Surgery on May 15, 2019
People with Carotid Artery Disease Are at Increased Risk

Stroke, or brain attack, can affect people of all ages and backgrounds. It is the No. 5 cause of death and a leading cause of disability in the United States.
A stroke occurs when a blood vessel that carries oxygen and nutrients to the brain is either blocked by a clot or bursts (or ruptures).
Every year, more than 300,000 Americans are diagnosed with blockages in their carotid (neck) arteries that carry blood to the brain. This condition can lead to a dangerous stroke.
To help protect members of our community at risk for strokes, the Stony Brook Vascular Center offers a safe, innovative procedure called transcarotid artery revascularization (TCAR).
This minimally invasive procedure treats carotid artery disease, and is clinically proven to protect against stroke both during and after the procedure.
Stony Brook has performed more TCAR procedures than any hospital on Long Island
Stony Brook was the first hospital on Long Island to offer this revolutionary procedure (read more).
Carotid artery disease is a blockage or narrowing in the arteries that carry oxygen-rich blood to the brain. These arteries are located in the neck, one on each side.
The blockage, caused by cholesterol-filled plaque, reduces the amount of blood that flows to the brain. Because the blood isn't flowing normally, blood clots can form or small pieces of plaque can break off and travel to the brain, causing a stroke.
Every year, 15 million people worldwide suffer a stroke, and carotid artery disease is estimated to be the source of the stroke in up to one third of patients.
There currently are multiple treatment options for stroke prevention. If the blockage or narrowing in the artery isn't severe, lifestyle changes and regular monitoring may be the only action required.
If the disease is more advanced, our vascular specialists provide three different treatments depending on the individual patient and degree of severity:
- The traditional open surgery, called a carotid endarterectomy, or CEA
- A minimally invasive procedure called transfemoral carotid artery stenting
- The state-of-the-art TCAR procedure that reduces the risk of stroke both during and after the procedure
Transcarotid artery revascularization is a minimally invasive treatment performed by going into the carotid arteries to restore the flow of blood to the brain (revascularization).
The procedure is a major advance in treating carotid artery disease. Here's how it's done:
- The procedure is performed with the patient under light sedation, in Stony Brook Hospital's hybrid operating room. It takes about 90 minutes.
- The surgeon makes a tiny incision at the neckline just above the clavicle. The scar is so small that most people never notice it.
- A tube, called a catheter, is placed directly into the carotid artery.
- The catheter is connected to a revolutionary system called a neuro-protection system (NPS). The NPS temporarily reverses the blood flow away from the brain. So, if any plaque breaks loose or blood clots form during the procedure, it won't go into the brain. This means that there is almost 100% protection from stroke while the rest of the procedure is done.
- A stent — a metal mesh tube — is implanted into the carotid artery. The stent expands and opens the artery for improved blood flow. It also stabilizes the plaque to help prevent future strokes.
- The patient's blood flow that was reversed is filtered to ensure there are no particles in the blood. The filtered blood is then returned through a second catheter in the upper thigh, and the flow reversal is turned off so the blood flows in the normal direction.
- After an overnight stay in the hospital to monitor blood pressure, the patient can go home and resume normal activities.
The stent that was placed in the artery stays in the body permanently, to keep the artery open and the blood flowing normally.
It has been shown that over ten years, the degree to which the artery stays open after the TCAR procedure is equivalent to the results of the CEA surgery. And because TCAR is less invasive than traditional surgery, there's a lower chance of complications.
"I can't emphasize how important this is in the field of vascular surgery," says Angela A. Kokkosis, MD, director of carotid interventions at the Stony Brook Vascular Center.
"It's a treatment revolution for people who are at risk for strokes because of carotid artery disease."
To determine eligibility for TCAR, there are very strict criteria based on Centers for Medicare and Medicaid Services (CMS) guidelines as well as guidelines from the company that developed TCAR.
Generally, patients who have never had a stroke and have blockage greater than 80% but less than 100% are good candidates for TCAR.
In addition, current guidelines are that TCAR may be right for patients with carotid artery disease who are considered high risk for traditional open surgery.
Factors that make a person high risk — meaning the open surgery is not a good choice for them — include older age, anatomic issues or previous cancers or surgeries that may make the carotid blockage surgically inaccessible, and other medical conditions such as severe heart or lung disease.
Stony Brook was the first hospital on Long Island to provide the revolutionary TCAR
TCAR is appropriate for patients of any age, though people who need carotid intervention are generally older. The average age of patients treated with TCAR recently at Stony Brook has been 75. The procedure is covered by Medicare.
After a stroke, many patients lose their quality of life. By reducing the incidence of strokes and the debilitation they can cause, TCAR can preserve quality of life for people with carotid artery disease.
Due to the excellent outcomes patients are experiencing from TCAR, it is expected that the guidelines for who can get the procedure will be expanded to include a broader range of people with carotid artery disease.
Stony Brook has performed more TCAR procedures than any hospital on Long Island, and we are second in New York State in terms of number of patients treated with TCAR.
At Stony Brook, TCAR is performed by Dr. Kokkosis as well as by her vascular colleagues, George J. Koullias, MD, PhD, Shang A. Loh, MD, and Apostolos K. Tassiopoulos, MD, chief of vascular and endovascular surgery.
| Non-Surgical Ways to Prevent Stroke: n Know and control your blood pressure n Don't smoke, or stop n Lose weight if overweight n Be active physically n Identify and manage atrial fibrillation n Treat a transient ischemic attack n Treat circulatory problems n Know and control your blood sugar and cholesterol n Drink alcohol in moderation, if at all n Eat a healthy diet low in sodium and rich in potassium n Know the warning signs of stroke and respond immediately. |
Posted by Stony Brook Surgery on May 7, 2019
Mohs surgery — originally developed in the 1930s by Frederic E. Mohs, MD — has been refined into the most advanced, precise, and effective treatment for an increasing variety of skin cancer types.
With the Mohs technique, it is possible to precisely identify and remove an entire tumor while leaving the surrounding healthy tissue intact and unharmed.
While treatment of the skin cancer is a patient's primary concern, reconstruction of the treated area is also important. Once all of the cancer has been removed, surgeon and patient determine together if a reconstruction procedure is needed and what kind of procedure to use.
The surgeon may be able to tell whether the reconstruction should take place immediately after surgery or be delayed until later.
There are several options for post-Mohs reconstructive surgery available today. They vary because the locations, amounts, and types of tissues affected differ from person to person. The size of the tumor and depth of its roots are factors.
Here, Tara L. Huston, MD, a member of our Plastic and Reconstructive Surgery Division and leader of the Melanoma Management Team of the Stony Brook Cancer Center, answers frequently asked questions about post-Mohs reconstructive surgery after skin cancer.
Q: What exactly is Mohs surgery?
A: Mohs surgery is the most precise way to remove a basal or squamous cell skin cancer. The dermatologic surgeon cuts out (excises) the cancer layer by layer, looking at the tissue that is removed under the microscope until the absence of all cancer cells is confirmed.
Mohs surgery offers the highest potential for cure, even if the skin cancer has been previously treated by another method.
Basal and squamous cell skin cancer — the two most common kinds of skin cancer — occur on the outer layer of the skin. They are most often found in areas exposed to the sun, such as the head, neck, and arms, but they also can occur elsewhere.
In recent years, Mohs surgery is being increasingly used as an alternative to standard excision for certain melanomas. However, not all doctors agree on using Mohs for melanoma, which is the most dangerous form of skin cancer and can penetrate the skin deeply.
Our specially-trained Mohs surgeons have a state-of-the-art unit
designed especially for Mohs surgery, with all the latest technology needed for it.
Q: Why is Mohs surgery so effective in treating skin cancer?
A: With the Mohs technique, as compared to traditional surgical removal of skin cancer, more of the specimen is able to be evaluated under the microscope. This is the best way to ensure that all of the cancer cells have been removed. The effectiveness of Mohs is near 99%, while traditional surgical removal is slightly lower.
Q: What areas of the body are treatable by Mohs surgery?
A: As Mohs is a tissue-preserving technique, it is most commonly used on areas that are of high functional and aesthetic importance such as the head, neck, hands, feet, and anogenital region.
Q: What is reconstruction following Mohs surgery?
A: The goal of reconstruction following Mohs surgery is to restore form and function to the areas which were treated for skin cancer. For this part, the dermatologic surgeons will often work in concert with plastic surgeons.
Q: What are the options for reconstruction after Mohs surgery?
A: The options for reconstruction depend on the anatomic location, depth, and extent of the Mohs defect. Reconstruction can be as simple as guiding wound healing and allowing the area to contract on its own.
Sometimes the defects can be closed in a straight line. Other times a skin graft is used (from near the ear or clavicle) or the local tissue is rearranged.
In rare instances, free-tissue transfer (from a distant part of the body) is done. Our surgeons are skilled in this technique as well. The plastic surgeon will attempt to hide the scars along existing facial creases and natural landmarks for the most aesthetic result.
Q: When is reconstruction done after Mohs surgery?
A: Reconstruction is most commonly performed the same day or the day following the Mohs procedure.
Our plastic surgeons are highly skilled at performing the full range of
post-Mohs reconstructive procedures, and they work closely with our Mohs surgeons.
Q: How are the different reconstructive procedures done?
A: The great majority of the procedures discussed here are performed in the plastic surgeon's office under local anesthesia. Only a small handful of the cases that we do here at Stony Brook Medicine require a trip to the operating room. This can either be for patient comfort or to close a very large defect.
Q: What is the recovery time for each of these procedures?
A: With most of these reconstructive procedures, the downtime is minimal. Most patients are able to be back to their normal activities by the following day wearing just a band aid. In most cases, over the counter acetaminophen (Tylenol) is sufficient to control the associated discomfort.
Q: Is post-Mohs reconstructive surgery considered cosmetic or medically necessary?
A: When referred by the dermatologic surgeon for post-Mohs reconstruction, most insurance companies consider it medically necessary and do cover the cost of the procedures.
Q: What is the advantage of having post-Mohs reconstructive surgery done at Stony Brook Medicine?
A: Stony Brook Medicine provides comprehensive, multidisciplinary care to patients with skin cancer. We offer screening, surgery, and the option to participate in clinical trials. The availability of clinical trials serves as a hallmark of our ability to offer leading-edge treatment.
Our specially-trained Mohs surgeons have a state-of-the-art unit designed especially for doing Mohs surgery, with all the latest technology needed for it.
Our plastic surgeons are highly skilled at performing the full range of post-Mohs reconstructive procedures, and they work closely with our Mohs surgeons.
Our dedicated team of dermatologists, dermatopathologists, surgeons, medical oncologists, and radiation oncologists meets frequently to review cases, and thus we ensure our patients receive all the benefits of multidisciplinary care.
| FREE Skin Cancer Screening and Melanoma Educational Program provided by Stony Brook Medicine Dermatologists and Melanoma Team: When: Saturday, May 11, 8 to 11:30 am. Where: 23 South Howell Avenue, Suite G, Centereach, NY 11720 (map/directions). Are you 18 or older? Was your last skin cancer screening by a dermatologist more than a year ago? If so, call 631-444-4000 for an appointment. |
Posted by Stony Brook Surgery on April 30, 2019
Skin cancer — including melanoma as well as basal and squamous cell carcinomas — is the most common of all cancer types.
The American Cancer Society estimates that in the United States this year there will be about 96,480 new cases of melanoma, the most dangerous form of skin cancer, and 7,230 deaths from it. The rates of melanoma have been rising for the last 30 years.
The number of cases of the more frequent skin cancers, basal cell carcinoma and squamous cell carcinoma, has been increasing for many years. According to one estimate, about 3.5 million cases of them are diagnosed annually (80% are basal cell).
Most of these three types of skin cancer are caused by exposure to ultraviolet (UV) light primarily from the sun. However, only a little over half of American adults use sun-protection measures.
The good news is that if diagnosed and treated early, skin cancer can often be cured. But if the disease is allowed to progress, it can result in disfigurement and possibly death.
Here, Tara L. Huston, MD, associate professor of surgery and dermatology, and leader of Stony Brook's Melanoma Management Team, explains what can be done to help prevent skin cancer and how to detect its early signs.
May is National Skin Cancer and Melanoma Awareness Month.
Q: What should people know about protecting themselves against skin cancer?
A: Skin cancer is usually the result of sun exposure and blistering sunburns that occur in childhood in addition to cumulative sun exposure. The most important thing we can do is to protect our children from early sun exposure, although it's never too late to reduce your own risk for skin cancer. Eliminating ongoing sun damage is very important.
The good news is that most people with skin cancer are going to be fine. The majority of skin cancers are either basal cell or squamous cell carcinomas. Only 4% of all skin cancers are melanoma, the most serious type of skin cancer.
Q: Besides early sun exposure, what are some other risk factors for skin cancer?
A: Skin type has a lot to do with it. Fair skin, light hair, and light eyes are risk factors for melanoma. Sun exposure is by far the most common risk factor. The use of tanning salons is also a risk factor. Self-tanning lotions do not pose a risk.
Q: What are the symptoms of skin cancer, and what should people look for?
A: ABCDE is the key. This applies to new or changing moles. A is for asymmetry; B is for irregular borders; C is for color variation; D is for a diameter greater than 6 millimeters (about the size of a pencil eraser); and E is for evolution, or any change in a mole, including itching or bleeding. Any new lesion that bleeds or scabs and does not go away over four weeks should be brought to your physician's attention.
When in doubt about a mole, get it checked out … What to look for.
Q: How often should people do self-body checks for changing moles, and how often should they get clinical checkups?
A: People should be aware of their skin and look for any changing moles on a daily basis. People who don't have any history of skin cancer should have a total body skin examination annually by a physician.
People with a history of skin cancer, especially melanoma, should be evaluated at least twice a year by a dermatologist and do skin self-checks monthly. It's a lifetime of follow-up evaluations with your doctor, not just because of possible melanoma recurrence, but because of the possibility of other skin cancers as well.
Q: How can people protect themselves against the UVA and UVB rays of the sun?
A: Plan your outdoor activities before 10 am and after 4 pm. Use a broad-spectrum sunscreen with SPF of 30 or higher, and apply over all exposed skin about ten minutes before going out, and reapply every two hours, or sooner if swimming.
There is also clothing that now has UV protection in them, including bathing suits for kids. And be sure to wear a hat to protect the scalp and ears. Sun-exposed areas such as the nose and ears are very common spots where skin cancer can develop.
Q: How is skin cancer treated?
A: If you have a lesion that you're worried about, the first step is to see a board-certified dermatologist, who will remove it if it looks suspicious. Most of the basal and squamous cell cancers are handled with local removal by a dermatologist or plastic surgeon, and that's all the treatment needed.
When outside, seek shade, cover up, wear a hat and sunglasses, and use sunscreen.
If there is a diagnosis of melanoma, a melanoma surgeon will become involved, and the treatment depends on the depth of the melanoma.
If it's what we call a thin melanoma, which is less than one millimeter deep (1/25 of an inch), the treatment is removal with a margin of normal skin around the melanoma.
Once the melanoma is more than one millimeter deep or demonstrates concerning features on pathology exam, we also sample the lymph node, because the deeper the melanoma, the greater the chance of lymph node involvement.
Q: What distinguishes Stony Brook from other centers in treating skin cancer?
A: Stony Brook provides comprehensive, multidisciplinary care to patients with melanoma. We offer screening, surgery, and the option to participate in local and national clinical trials. In addition, we conduct basic science and translational research, and also provide community education.
While clinical trials are not for everyone and participation in them is strictly voluntary, the availability of these trials serves as a hallmark of our ability to offer leading-edge treatment.
Several trials are currently underway at Stony Brook. We recently participated in the Multicenter Selective Lymphadenectomy Trial (MSLT 2) that evaluated the role of completion lymph node surgery in melanoma, in order to determine the optimum care for patients (see Dr. Huston's blog about it).
Our dedicated team of pathologists, dermatologists, medical oncologists, and melanoma surgeons meets once a month to review each melanoma case, and thus ensures that our patients receive the benefits of multidisciplinary care.
Editor's note: Dr. Huston and her fellow melanoma surgical specialists, Alexander B. Dagum, MD, Christopher S. Bellber, MD, and Aleksandra Krajewski, MD, bring years of experience and excellent outcomes to the management of skin cancer.
|
FREE Skin Cancer Screening and Melanoma Educational Program provided by Stony Brook Medicine Dermatologists and the Melanoma Management Team:
When: Saturday, May 11, 8 to 11:30 am. Where: 23 South Howell Avenue, Suite G, Centereach, NY 11720 (map/directions). Are you 18 or older? Was your last skin cancer screening by a dermatologist more than a year ago? If so, call 631-444-4000 for an appointment. |
For more information about skin cancer and its prevention, please visit the Centers for Disease Control and Prevention. Another good online resource is the Skin Cancer Foundation.
Posted by Stony Brook Surgery on April 16, 2019
Our Voice Specialists Are Here to Help You Take Care of Your Voice
Every year in April, otolaryngologist–head and neck surgeons — commonly called ENT doctors — and other voice health professionals worldwide join together to recognize World Voice Day. It's April 16.
World Voice Day, which was established 17 years ago, encourages men and women, young and old, to assess their vocal health and take action to improve or maintain good voice habits.
The long-term consequences of poor voice care can range from strained vocal cords and chronic hoarseness to deadly head and neck cancers.
The voice specialists of our Otolaryngology–Head and Neck Surgery Division — otolaryngologist-laryngologist Melissa M. Mortensen, MD, otolaryngologist Joshua M. Rosenthal, MD, and speech pathologist Marilyn D. Baricevac, MS, CCC-SLP — provide a range of services aimed at vocal health and wellness.
A singer's voice is a musical instrument and the special care it needs
can be applied to everyone who wants to have a healthy voice.

Here, Dr. Mortensen offers tips on how singers can ensure that their voice stays healthy throughout their career:
1. Think of yourself as a vocal athlete. Just like an athlete, it is important for a singer to receive the proper training regarding technique and use. It is important to not overuse the voice. It is important to get plenty of rest, eat a well-balanced diet, and get plenty of hydration. Just like professional athletes who spend hours perfecting their abilities, it is important for the singer to have the same disciplined practice schedule with intervals of rest and recovery to perform at an optimal level, regardless of genre.
2. Warm-up. Just as the athlete stretches it is important to have exercises to stretch-out your vocal muscles or warm-up. Every singer always needs a good vocal warm up before they sing, whether practicing or getting ready to go on stage, a good warm up is vital. Many new or inexperienced artists risk doing permanent damage to their vocal folds because they are unaware of the importance of doing a warm-up before they sing
3. Hydration, hydration, hydration. It is important to be well hydrated for any singer. Drinking non-carbonated and non-caffeinated drinks helps the mucous that coats the vocal folds to act as a lubricant. Most experts recommend 8-10 eight-ounce glasses of water daily to ensure this. Otherwise, you could find yourself with a dry scratchy throat, the need to clear your throat more often and find you require more effort to use your voice.
4. Be an original. You want your voice to be the next big thing and not be a copycat. Trying to imitate another singer's style could put undue pressure on your vocal folds and you may then sing or do things outside of your comfortable physiologic range or current vocal skill level. This could result in vocal injury. Let your style speak or sing for itself.
5. Optimize your schedule. Just like an athlete before the big game, you should not cram all of your preparation for your shows and auditions at once. An athlete would not try to prepare for the big game by practicing all in one day and neither should you. You should sing in small increments daily, about 30-45 minutes, until you have worked on building your muscular skill and stamina. As you improve you can increase the length of time and vocal difficulty of the pieces you are working on.
6. Avoid activities that cause trauma to your vocal folds. These include the obvious such as yelling and screaming and the not so obvious, prolonged speaking, speaking loudly, and singing loudly for prolonged periods of time. All of the above activities cause the vocal folds to bang together at a higher velocity. The immediate impact can be vocal fold swelling and irritation. The long-term impact can be vocal fold nodules.
7. Avoid alcohol and smoking. Smoking causes your vocal folds to be irritated. Constant irritation can lead to vocal fold edema which can lead to phonotraumatic problems. Alcohol can cause dehydration of the vocal folds so they don't vibrate effectively. Both alcohol and smoking can predispose you to acid reflux which can cause further swelling and injury to the vocal folds.
Like singers, everyone should protect their voice by drinking 6 to 8 glasses of water a day, limiting caffeine and alcohol, and avoiding tobacco smoke.
Many people don’t understand the signs and symptoms of voice disorders and often put off treatment, which can cause irreparable damage to their voice quality.
It's time to see an otolaryngologist when you have or suspect a voice problem and there are any of the following conditions:
|
Posted by Stony Brook Surgery on April 10, 2019
Educate Yourself on the Risk Factors, Signs, and Symptoms
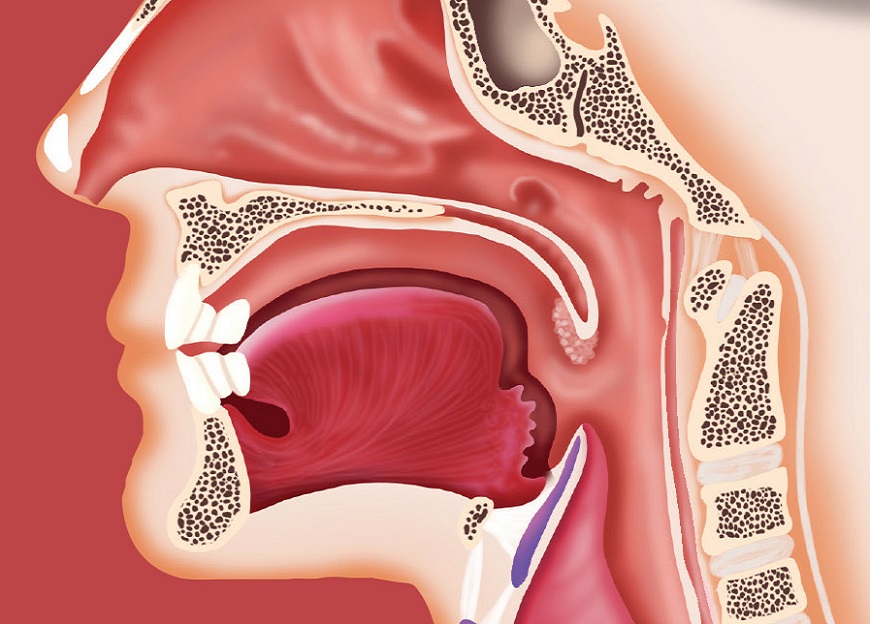
Approximately 53,000 people in the U.S. will be diagnosed this year with oral cancer (cancer of the mouth).
One hundred forty-five new people every day will be diagnosed with an oral cancer, and one person every hour of the day will die from it — that's nearly 9,000 deaths from oral cancer every year.
Of the people newly diagnosed with oral cancer, only about 60% will live longer than five years.
Moreover, many who do survive suffer long-term problems such as severe facial disfigurement or difficulties eating and speaking. The death rate associated with oral cancer remains high because the cancer tends to be discovered late in its development.
Oral cancer awareness in the American public is low. While smoking and tobacco use are major risk factors, the fastest growing segment of oral cancer patients is young, healthy, nonsmoking individuals due to the connection to the human papillomavirus (HPV). The only hope to save lives is public awareness.
Early cancer diagnosis saves lives. If detected early, oral cancer has an 80% survival rate. The most effective way to manage oral cancer is to combine early diagnosis with timely and appropriate treatment
The fastest-growing cause of oral, head and neck cancers is HPV. In fact, if you have HPV, you're 30 times more likely to develop oral cancer.
Oral cancer can be treated when detected early. People can learn how to examine themselves for possible signs and symptoms (see instructions). If one is detected, they should see their dentist, oral and facial surgeon, or other healthcare professional immediately.
Some of the most common oral cancer signs and symptoms include:
- Persistent mouth sore: a sore in the mouth that does not heal is the most common symptom of oral cancer
- Pain: persistent mouth pain is another common oral cancer sign
- A lump or thickening in the cheek
- A white or red patch on the gums, tongue, tonsil, or lining of the mouth
- A sore throat or feeling that something is caught in the throat that does not go away
- Difficulty swallowing or chewing
- Difficulty moving the jaw or tongue
- Numbness of the tongue or elsewhere in the mouth
- Jaw swelling that makes dentures hurt or fit poorly
- Loosening of the teeth
- Pain in the teeth or jaw
- Voice changes
- A lump in the neck
- Weight loss
- Persistent bad breath
If any of these oral cancer signs or symptoms are present for days or weeks, your doctor may recommend tests to check for oral cancer. As with any cancer, having your cancer diagnosed as soon as possible will help ensure that any treatment is as effective as possible.
| Free screening for oral cancer will be provided on Sunday afternoon, April 14, by the Stony Brook Dental Care Center team at the Spring Health Fair in Peconic on the North Fork (details). Early detection is key! Screening takes less than 10 minutes. A clinician looks over the inside of the mouth to check for white patches or mouth sores, feels the tissues in your mouth to check for lumps or other abnormalities, and may use a state-of-the-art non-invasive scope device that emits a harmless, bright blue light to see mouth tissue changes not visible under normal white light examination. |
Posted by Stony Brook Surgery on April 8, 2019
There has been a tremendous amount of talk about breast implants in the news and on social media recently. Last month, the Food and Drug Administration (FDA) convened an advisory panel to discuss the long-term benefits and risks of breast implants for both breast augmentation as well as reconstruction.
Breast implants have a decades-long history. The first "mammaplasty" procedure using implants — was performed in 1962. The implants, then, were a silicone rubber envelope-sac, shaped like a teardrop, which was filled with viscous silicone-gel.
Implants have evolved and improved over time. Now breast implantation is one of the most popular forms of plastic surgery done in the United States. In 1976, the FDA started to regulate silicone breast implants, subjecting them to controls and performance standards.
Here, Tara L. Huston, MD, associate professor of surgery and a member of our Plastic and Reconstructive Surgery Division, answers frequently asked questions about breast implants. The information she provides is essential for women who already have or are considering getting breast implants.
Q: What is the purpose of breast implants?
A: Breast implants are medical devices used to increase the size and change the shape of the breast. For women who undergo mastectomy for breast cancer, they are the most commonly used method of recreating a breast (reconstructive purpose). For women who desire larger breasts, they are placed behind the existing tissue to augment cup size (cosmetic purpose).
Q: What exactly is a breast implant made of, and what are the different types?
A: The breast implant shell is composed of silicone. The inside fill can be either saline (salt water) or silicone gel. From 1994 to 2006, the FDA did not allow the placement of silicone-filled implants in the United States for cosmetic purposes.
During this time, the FDA collected data and concluded that there was no increased risk of connective tissue disorders. Since 2006, both saline and silicone implants were permitted to be used for reconstructive and cosmetic purposes.
Q: What is the difference between a smooth and a textured breast implant?
A: The difference is in the appearance and feel of the shell. Smooth implants have a soft, uniform shell and tend to move more as the capsule doesn't grow into them. Textured implants have a coating, creating in a larger surface area, which causes the capsule to grow them and results in less movement.
Q: What complications can occur with the implants themselves?
A: Local complications include capsular contracture, malposition, and rupture. Some people also experience breast pain, wrinkling, asymmetry, scarring and infection.
Q: What conditions are associated with having breast implants?
A: Breast implant-associated anaplastic large cell lymphoma and an entity known as breast implant illness.
Q: What is anaplastic large cell lymphoma?A: Breast implant-associated anaplastic large cell lymphoma, known by the abbreviation BIA-ALCL, is a cancer of the immune system which is most often found in the capsule around the implant. It is NOT a breast cancer.
There have been 673 cases worldwide reported to date. While most patients with BIA-ALCL have been treated with only breast implant removal, some patients have required radiation therapy, chemotherapy, or both, and 16 patients have died from BIA-ALCL.
Incidence estimates are highly variable but range from roughly 1 in 3,000 patients to 1 in 30,000 patients with textured implants.
There are no confirmed cases of BIA-ALCL in women with smooth implants. BIA-ALCL has been reported in both silicone- and saline-filled implants. It is the textured shell that seems to be the issue, and not the fill.
If you have any issues, questions, or concerns, please arrange for a consultation with
one of our plastic surgeons to help you by calling our office at 631-444-8210.
Q: What does a woman with breast implants need to look out for in regard to BIA-ALCL?
A: BIA-ALCL usually develops as a swelling of the breast 2 to 28 years after the insertion of breast implants. It most commonly presents as a fluid collecting around the implant. It can also present as a lump in the breast or armpit. If a woman with implants notes that only one breast is enlarging, this is an indication to see a plastic surgeon for an evaluation.
Q: What is breast implant illness?
A: There are many breast implant patients on social media who discuss a wide variety of symptoms that they are experiencing — symptoms which may or may not meet the diagnostic criteria to be categorized as a disease.
These patients refer to their symptoms collectively as "breast implant illness." However, there currently is not sufficient evidence to demonstrate an association between breast implants and rheumatologic or connective tissue diseases.
Q: What is the follow-up needed for women with breast implants?
A: Once the plastic surgeon has established that a woman has healed, and her implants have settled, she does not need yearly follow-up just because she has breast implants. However, if the implants were placed for reconstruction following cancer surgery, we do ask patients to see their surgeons yearly.
Asymptomatic women without breast changes do not require more than routine follow-up with their primary physician or gynecologist for a yearly breast exam.
If a woman with breast implants experiences a change in her breasts — especially if there is swelling or a lump — she should undergo examination and appropriate imaging, including ultrasound and fine-needle aspiration of any peri-implant fluid.
The woman who understands the risks as well as benefits of breast implants, and knows
what danger signs to look out for, is the best possible breast advocate for herself.
Q: Does a woman with implants need frequent MRI exams to check them?
A: As of last week, the FDA's prior recommendation of MRI screening at three years after implant placement and every two years thereafter was called into question. A breast implant MRI study is rarely covered by insurance companies and only looks at the implant, not the surrounding breast tissue.
Even if a silent rupture is identified, most women will not undergo surgery if they are not experiencing issues.
The recommendations are moving toward ultrasound, beginning at least five years after the implants are placed.
Ultrasound is a good test to look for capsule thickening and peri-implant fluid. If there is a silent rupture suspected on ultrasound, an MRI can further characterize but it is no longer considered the first-line imaging test for screening.
Q: Does having implants change a woman's breast cancer screening?
A: No. It is still recommended that women have a baseline screening mammogram at age 35 and then begin yearly mammograms at age 40. If you have dense breasts, a yearly ultrasound may be recommended in addition.
Q: Is there an expiration date on current breast implants?
A: No ten-year "time limit" exists at which time implants expire and must be removed or replaced. If a woman with breast implants is not experiencing issues, it is unlikely she will need to have another operation.
Q: If a woman wants to remove her breast implants, will health insurance cover the procedure?
A: Breast augmentation is considered cosmetic, and is not covered by insurance companies. As such, removal of breast implants also is not commonly covered by insurance companies. An exception is in the case of previous or current cancer diagnosis for which they will often cover implant surgery.
Q: What is the take home message for women who already have or are considering getting breast implants?
A: Breast implants are not lifetime devices. They will likely require maintenance such as an additional operation at some point. The longer a woman has breast implants, the more likely she is to experience local complications or adverse outcomes requiring re-operation.By being an informed consumer, understanding the risks as well as benefits, and knowing what danger signs to look out for, a woman with breast implants is the best possible breast advocate for herself!
Posted by Stony Brook Surgery on April 4, 2019
We Are Leading the Way in Patient Care with Leading-Edge Technology
The Suffolk County Volunteer Firefighters Burn Center of University Hospital — the only designated burn care facility in Suffolk County — has recently acquired state-of-the-art laser technology for treating burn scars, called UltraPulse SCAAR FX.
This fractional CO2 laser has emerged in recent years as the premier tool for improving the texture and elasticity of severe burn scars.
The SCAAR FX laser technology allows for advanced treatment of a variety of severely damaged skin lesions that require synergistic coagulation and ablation for advanced resurfacing (hence, SCAAR).
"We are very pleased we can now offer laser therapy to modify burn scars when they occur," says Steven Sandoval, MD, assistant professor of surgery and medical director of the Burn Center, who led the initiative to acquire the SCAAR FX laser.
"For the last several years we have had to send patients to Nassau University Medical Center in neighboring Nassau County, and as far as Shriners Hospital in Boston, for this type of scar management.
We are the first in Suffolk County to offer SCAAR FX laser treatment for burn scars.
"Now we have, for the first time in Suffolk County, the ability to offer this care to improve range of motion, quality of life, and overall functionality."
For these reasons, the advanced laser technology that makes SCAAR possible is a welcome addition to the world-class care that Stony Brook University Hospital provides to the people of Suffolk County.
SCAAR FX laser treatment is minimally invasive, compared with surgical scar revision. It offers patients an attractive new option. Its power and precision enable Dr. Sandoval to customize treatments for all degrees of burn scars, from small to the most severe, with optimal comfort and healing time.
SCAAR FX uses a unique ablation/coagulation ratio to substantially improve the structure of deep contracted lesions by restoring more normal collagen deposition. This maximizes results, minimizes thermal damage, and reduces treatment time.

| A) Patient's hand following severe burn injury and subsequent skin grafts, showing residual hypertrophic scars — raised, thick, wide — with worst scar contracture (tightening of healed skin) patient had experienced. B) Hand after series of four treatments with SCAAR FX, showing reduction of scar tissue. Marked improvement in scar flexibility and functionality of hand was observed. (Click on image to enlarge.) |
SCAAR FX creates a pattern of small microscopic channels that break down the stiffness of the scar and triggers production of restored tissue representing normal skin.
The result is deep dermal regeneration that dramatically improves the elasticity and appearance of the patient's scar back toward normal skin.
When it comes to improving the smoothness and the little elevations that are so bothersome to the burn patient, and especially when it comes to the stiffness of the scar, the SCAAR FX laser has no competition, according to several experts in the field of burn care.
Recently, a panel of eight prominent American academic and military dermatologists and plastic surgeons with extensive experience in laser treatment of scars published a consensus report in JAMA Dermatology that concluded "laser scar therapy, particularly fractional ablative laser resurfacing, represents a promising and vastly underused tool in the multidisciplinary treatment of traumatic scars."
The Suffolk County Volunteer Firefighters Burn Center has approximately 200 inpatient admissions per year, with more than 1,500 clinic appointments last year. It is designed and equipped to meet the special needs of burn patients, and is certified by the American Burn Association. The original center, an eight-bed unit, was established in 1985.
The Burn Center quickly gained the enthusiastic backing of the volunteer firefighters of Suffolk County, who soon after the establishment of the Burn Center created the Suffolk County Volunteer Firefighters Burn Center Fund to help support special clinical and research initiatives. The Burn Center was renamed in 2013 in honor of their dedicated support of it.
| "Despite expert wound care and assiduous management with traditional therapy, poor cosmetic outcomes, restricted motion, and symptoms such as pain and itch are a pervasive problem of disfiguring and debilitating scars. The advent of ablative fractional photothermolysis [laser resurfacing] within the past decade and its application to the treatment of traumatic scars represents a breakthrough in the restoration of function and cosmetic appearance for injured patients, but the procedure is not widely used.… Changes to existing scar treatment paradigms should include extensive integration of fractional resurfacing and other combination therapies guided by future research." — "Consensus Statement," JAMA Dermatology (see article) |
Posted by Stony Brook Surgery on March 26, 2019
New Study Finds Encouraging Results for Patients with Low Surgical Risk for Aortic Valve Replacement
Stony Brook University Hospital, in 2012, was the first hospital in Suffolk County to offer a newly FDA-approved procedure to treat severe aortic stenosis (narrowing of aortic valve opening) by replacing the aortic valve with a prosthetic valve, without the need for open heart surgery.
Called transcatheter aortic valve replacement, or TAVR, this minimally invasive treatment offers new hope for high-risk patients with severe symptomatic aortic stenosis in need of lifesaving valve replacement surgery. Since 2012, Stony Brook has acquired one of the most experienced heart teams for TAVR in the region.
Use of TAVR in patients deemed at low risk for conventional surgical valve replacement is now being studied, and Thomas V. Bilfinger, MD, ScD, professor of surgery and a leader of the Stony Brook Heart Institute has been participating in multicenter clinical trials of it.
Here, Dr. Bilfinger explains the latest findings of one of these trials just published online in the American College of Cardiology's journal Cardiovascular Interventions, under the title "Transcatheter Aortic Valve Replacement in Low-Risk Patients: One-Year Results from the LRT Trial" (see abstract).
Traditional aortic valve replacement requires a sternotomy to open the chest and a choice between a mechanical or a tissue valve. In recent years overwhelmingly most surgical aortic valve replacements (SAVRs) were done with bioprosthetic tissue valves.
Minimal surgical approaches with partial sternotomies or parasternal incisions were used more frequently but overall the operation, although much safer than in the beginning, has not drastically changed.
A fundamentally new approach was introduced with transcatheter aortic valve replacement (TAVR) where a tissue valve is crimped in such a way that it can be loaded on top of a catheter and be inserted through a groin artery and then be deployed covering the problematic native valve and pushing it aside.
Initially TAVR was tried out on very high-risk surgical patients. The feasibility of this new treatment approach was established with the PARTNER (Placement of AoRTic TraNscathetER) trial, a large multicenter trial initiated earlier in the present decade.
The appeal of TAVR is no surgical incision, less pain, a shorter or
no ICU stay, and faster return to normal activity.
Subsequently, in view of the positive outcomes, Medicare allowed this valve to be used on (and covered for) intermediate-risk patients. The patients have to be 65 or older, and fall into an intermediate-risk category calculated by the risk score developed by the Society of Thoracic Surgeons.
This is where we currently stand for Medicare to pay and, hence, most other commercial insurances.
Recently at a meeting in New Orleans, two significant studies were presented. Both studies were sponsored by valve manufacturers, and were evaluating TAVR in low-risk patients versus SAVR.
These studies completely flipped traditional thinking. It used to be that TAVR was considered for patients who were poor surgical candidates.
The early results from the subsequent PARTNER trial (PARTNER 3) suggest that TAVR should be the first choice, and SAVR should only be offered for patients that are not good TAVR candidates.
The PARTNER 3 trial was sponsored by the manufacturer of a TAVR system (Edwards) and randomized 1,000 patients to SAVR vs TAVR. Low surgical risk is defined as less than 4.0 % predicted mortality. The mean score was 1.9% and the average age was 73.
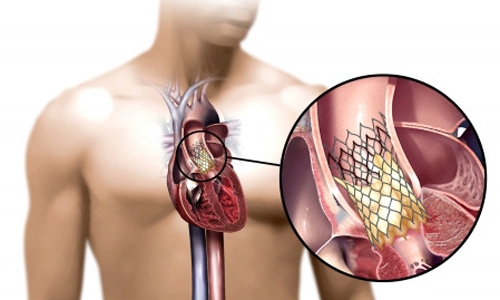
| Placement of the valve device is done from within the aorta, via catheter, without open heart surgery. |
At one-year follow-up, 8.5% of TAVR and 15.1% of SAVR met the primary composite endpoint of death, stroke, or rehospitalization. The one-year results for death or disabling stroke were 1.0% for TAVR and 2.9% for SAVR.
The second study was sponsored by the manufacturer of another TAVR system (Medtronic) and used a low-risk cutoff of less than 3.0%. It looked at two-year follow-up of 1,403 patients who underwent TAVR versus SAVR.
At two years they found that the all-cause death or disabling stroke rate was 5.3% for TAVR and 6.7% for SAVR, showing non-inferiority for TAVR. One thing that turned out to favor SAVR is the lower need for pacemakers than for TAVR.
Stony Brook has been involved in the two Low Risk TAVR (LRT) trials — LRT-1 and LRT-2 — organized by MedStar Washington Hospital Center in Washington, DC. These trials are not industry-sponsored, and allow use of both commercially available valves.
LRT-1 is not a randomized trial comparing SAVR versus TAVR, but more a "real world" experience of the use of these two valves in low-risk patients. Two hundred patients were enrolled with a mean age of 73.6 years.
At 30 days there was zero mortality, and zero strokes were observed. At one year the mortality was 3.0%; the stroke rate was 2.1%; and the need for a pacemaker 5.0%. These results at 30 days and at one-year follow-up are equally impressive.
LRT-2 is looking at leaflet thickening of these valves which may influence durability. When the valve leaflets become thickened and stiff, they may cause narrowing of the valve opening.
Durability is the crux of this whole field. SAVR valves have a life expectancy of 10-15 years and, at present, it is not known if TAVR valves last that long; hence, the reluctance of Medicare and the commercial insurances to pay for TAVR valves in low-risk patients with long life expectancies.
New data like the data presented with these trials may shift the paradigm, but in the end, like most things, the market will decide the place of TAVR.
At present at Stony Brook as in many other U.S. hospitals, TAVR has taken over from SAVR, though both procedures are offered on a daily basis.
| "Transcatheter aortic valve replacement (TAVR) is an established therapy for patients with symptomatic severe aortic stenosis (AS) who are extreme, high, or intermediate risk for surgical aortic valve replacement (SAVR). How TAVR compares to SAVR in patients who are low risk for surgery is now the subject of multiple clinical trials. The LRT trial was the first Food and Drug Administration-approved Investigational Device Exemption trial in the US to evaluate feasibility of TAVR in low-risk patients. Early results of the LRT trial confirmed safety of TAVR in low-risk subjects with symptomatic severe AS." — "Transcatheter Aortic Valve Replacement in Low-Risk Patients" (2019) |
Learn more about the Stony Brook Heart Institute's TAVR program. For consultations/appointments with our TAVR specialists, please call 631-444-1820. Watch this video (5:22 min):
Posted by Stony Brook Surgery on March 22, 2019
Coronary artery disease (CAD) is caused by plaque buildup in the wall of the arteries that supply blood to the heart; namely, the coronary arteries. Plaque is made up of cholesterol (fat) deposits. For some people, the first sign of CAD is a heart attack.
CAD is the leading cause of death for both men and women in the United States, and every year about 735,000 Americans have a heart attack, according to the Centers for Disease Control and Prevention.
Surgery (coronary artery bypass grafting, or CABG) has long been the gold standard treatment of advanced CAD. Blood is re-directed with arteries and veins to increase blood supply to the heart muscle.
Stents (tube-shaped metal devices) placed by cardiologists are ideal to open up blocked coronary arteries.
Stents provide very good results in patients with less advanced forms of CAD, and are the best emergency treatment for heart attacks. They are placed using a non-surgical procedure known as angioplasty or percutaneous coronary intervention (PCI).
HCR offers patients with multi-vessel CAD the benefits of both bypass surgery and stenting.
Bypass surgery is associated with extended survival, long-lasting relief of chest pain, improved exercise capacity, and minimizing the impact of heart attacks. Patients stay four to seven days in the hospital after bypass surgery, and return to normal activities and/or work in two to three months.
The benefits of PCI are not as long-lasting. However, recovery time after a PCI is short. Patients go home the day after the procedure, and usually can return to normal activities and/or work in seven to ten days.
A promising treatment option for some patients who have blockages in the artery of the front of the heart (left anterior descending artery) and at least one other blockage is a combination of both surgery and stenting, called hybrid coronary revascularization (HCR; revascularization means restoration of blood flow).
First performed in 1996, HCR gained traction toward the end of the first decade of the present century. An increasing number of these procedures are being done now by cardiac surgeons and cardiologists who work together as a team, and who have advanced the technique of doing it.
Here, Jorge M. Balaguer, MD, associate professor of surgery, who is a member of our Cardiothoracic Surgery Division and a leader of the Stony Brook Heart Institute, answers frequently asked questions about HCR in which he has a special interest and expertise. Dr. Balaguer has performed some of the pivotal research showing the safety and effectiveness of HCR.
Q: What is hybrid coronary revascularization, or HCR?
A: HCR is a heart operation that combines coronary bypass surgery with the placement of stents in coronary arteries via a non-surgical procedure. It requires the collaboration of cardiologists and cardiac surgeons to perform it.
The bypass procedure is minimally invasive, using a 2-3 inch incision between the ribs (no bone is divided) on the left side of the chest. This allows the surgeon to perform the bypass graft responsible for extended survival. It has a shorter recovery compared to conventional bypass surgery.
The other blocked arteries are treated with stents that release blood-clot preventing drugs to maximize their effectiveness.
Q: What are the benefits of HCR?
A: HCR offers patients with multi-vessel CAD the benefits of both bypass surgery and stenting. It is minimally invasive, and it does not compromise long-term durability and survival. It integrates the positive features of both CABG and stenting. Currently, it is provided only at a few select medical centers nationwide, including Stony Brook Medicine.
Additionally, benefits of HCR generally are shorter hospital stay, less pain after treatment, less scarring, and faster recovery — benefits that appeal to patients. Indeed, the benefits associated with HCR make treatment of CAD easier to face and easier to undergo.
Q: How is HCR performed? Are surgery and stenting done at the same time?
A: HCR can be performed at one time ("one-stop shop") in an operating room designed for both cardiovascular surgery and PCI stenting, called a hybrid operating room.
Most commonly, HCR is performed in a staged fashion. First, the minimally invasive bypass component is done in a traditional OR and then, after one or two days, the PCI with stent placement is done in a catheterization room.
Q: Must the heart be stopped, as in traditional bypass surgery, to perform HCR?
A: Most of time it is not necessary to stop the heart. The operation is generally performed "off-pump" — without the use of the heart-lung machine to take over the heart's pumping work — and eliminates the need to stop the heart. The surgical component of HCR is minimally invasive. These are the fundamental reasons for the very quick recovery.
Q: How long does the combined HCR procedure usually take?
A: The surgical component takes about three hours. The placement of the stents depends on how many are required. In general, it takes between one and two hours.
Q: How long after HCR can a patient to return to normal activity?
A: Most patients can get back to normal activity in about 3 to 4 weeks. They are discharged home after the procedure in four days or so, and are authorized to drive in seven to ten days.
Q: Has HCR been proven to be as safe and effective as CABG?
A: Yes. Several publications have shown that HCR is a safe procedure. Our own research looked at safety in great detail. It is necessary for the team to be thorough in the selection of patients and for careful planning to be done in the sequence of the surgery and the stenting. Management of some of the medications, especially blood thinners, around the HCR is very important in order to minimize bleeding complications and ensure good functioning of the stents.
Our hybrid ORs make HCR safer and easier in a variety of ways for both patients and physicians.
Q: What are the risks associated with HCR, compared with CABG?
A: Most scientific articles, including our own research and recent publications, show that the risks of HCR are comparable to those associated with conventional CABG. More attention to detail is required in the performance of the surgical component. The sequence of the stenting — before, at the same time, or after the bypass surgery — needs to be individualized to each patient.
Q: What qualifies a patient to be treated with HCR?
A: The anatomy of the coronary artery and the nature of the blockages are the initial determinants. Cardiologist and cardiac surgeon both need to agree that HCR can be performed. Candidacy also needs to be established in view of urgency, chest wall shape, and previous interventions, among other criteria.
Q: Does HCR require a special kind of operating room?
A: No, not necessarily. If the HCR is planned to be done at the same time, the hospital must have a hybrid OR, with capabilities for cardiovascular surgery as well as PCI stenting. Otherwise, the surgery can be done in a traditional cardiac OR, and the stenting a day or two later in a separate catheterization room.
Q: What is the advantage of having HCR done at Stony Brook Medicine?
A: The great collaborative relationship between cardiologists and cardiac surgeons at the Stony Brook Heart Institute makes HCR possible, as the performance of HCR requires teamwork to be successful. This well-established multidisciplinary care model is a major advantage.Another important advantage is the experience we bring to providing HCR, as demonstrated by our pioneering work in HCR and our outstanding track record in bypass surgery, which earned us the highest star rating for outcomes and quality from the Society of Thoracic Surgeons. These attributes are critical components of our HCR program at Stony Brook.
In addition, in the near future we will be performing the surgery part of HCR will the assistance of a surgical robot, which generally minimizes the stress of the bypass surgery. The robotic-assisted approach for HCR involves just three or four incisions less than one-half inch wide.
Currently, our new hybrid ORs, which feature the most up-to-date, technologically sophisticated equipment, enable what I like to call the "one-stop shop" HCR in which both surgery and stenting are done at the same time. This offers patients the advantage of having to undergo a single treatment experience.
Beyond that, our hybrid ORs make HCR safer and easier in a variety of ways for both patients and physicians. They are especially designed to do this.
| "Hybrid coronary revascularization for double-vessel coronary disease is associated with similar short-term outcomes and intermediate-term survival as traditional coronary artery bypass grafting. Hybrid coronary revascularization is associated with lower transfusion requirements and a shorter length of stay than coronary artery bypass grafting.… The excellent short-term and midterm clinical outcomes in these patients support the continued use of a hybrid revascularization strategy for patients with double-vessel coronary disease with appropriate angiographic anatomy." — Journal of Thoracic and Cardiovascular Surgery (2018; see abstract) |
Posted by Stony Brook Surgery on March 15, 2019
Our VAD Program Is Only on LI to Be Continuously Certified by Joint Commission since 2011

Joseph's incredibly active life had turned into constant fatigue, and he often had to sit down and rest at work. "Then it started to become harder to go up the stairs. It became more difficult, and harder to breathe," Joseph says.
The advanced heart specialists at Stony Brook's Heart Failure and Cardiomyopathy Center optimized Joseph's medications and explained his options. "In one day, I got a bunch of news I didn't want to get," Joseph recalls. "But Stony Brook fixed me up."
Allison J. McLarty, MD, surgical director of the ventricular assist device (VAD) program at Stony Brook University Heart Institute, performed surgery on Joseph to implant a VAD in early 2017.
The pump took over for his failing heart until he received a heart transplant on his 58th birthday — May 15 of 2018.
"For Joseph's treatment of advanced heart failure, the VAD served as a ‘bridge to transplant' — a lifesaving intervention that allowed him to become eligible to receive a heart transplantation," says Dr. McLarty.
"In one day, I got a bunch of news I didn't want to get," Joseph Cerqueira recalls. "But Stony Brook fixed me up."
"The implanted VAD took over the pumping work of the heart, allowing Joseph to become stronger and physically better prepared to undergo heart transplant surgery."
Today Joseph is back to work as executive chef at the catering facility Terrace On The Park, located in Queens. He supervises four kitchens that supply meals for 11 catering rooms plus a penthouse. It's a hectic life, but he loves it.
"I'm ecstatic about getting back to work. For me, it has been part of the healing process," Joseph says. "I wanted to work so I wouldn't be cooped up at home, staring at the walls."
His active schedule is a long way from the fatigue he experienced before the VAD implant. "Now my quality of life is perfect. I still get tired and I know my limitations, but besides that I do whatever has to be done."
Joseph is "extremely pleased" with the care he received from his surgeon Dr. McLarty; his cardiologist, Hal A. Skopicki, MD, PhD; and all the Stony Brook Medicine personnel he has encountered.
Joseph was diagnosed with severe heart failure after two heart attacks, and also learned he had type 2 diabetes.
"What can I say — they were more like friends or family," Joseph says. "Everybody went the extra mile to make me comfortable and knowledgeable on how to adapt to every aspect of life with a VAD."
"The care doesn't end after a patient receives a VAD," says Dr. Skopicki, chief of cardiology, Stony Brook Heart Institute; director, Heart Failure and Cardiomyopathy Center, and medical director, VAD Program. "Our VAD team explains every nuance involved with the device so the patient has the knowledge and confidence to leave the hospital and adjust to life at home."
At work he supervises other chefs, but when he's at home in Coram, Joseph loves to do the cooking. He is originally from Portugal, but was trained in Italy in a variety of cuisines: classical Italian, Greek, Middle Eastern, German, and Asian.
"So pretty much I can dabble in most everything," he says. "But I prefer Northern Italian. It's awesome." He especially likes to cook polentas, anything with legumes, hearty soups and fish.
He enjoys spending time with his wife Ivone and daughter Kimberly. He and Ivone plan to fly home to Portugal soon, to visit relatives there.
Once a month, Joseph attends the same support group for Stony Brook VAD patients that he went to when he was a heart patient. Now his purpose is to encourage others who are candidates for the device.
It's his way of "paying back" for the new life he's been enjoying since his VAD implant and subsequent heart transplant, he says. "So when people see me they can say, ‘Wow, this guy was once like me and now he's like this.' It gives people hope."
| When patients with advanced heart disease experience poor quality of life despite the best that medical therapy can offer, our team of specialists at Stony Brook Heart Institute's ventricular assist device (VAD) program can evaluate patients to see if they may benefit from implantation of state-of-the-art mechanical cardiac assist devices. A testament to the high-quality care of our patients, our VAD program is the only on Long Island to be continuously certified by the Joint Commission since 2011. |
Posted by Stony Brook Surgery on March 6, 2019
DVT Claims More Lives Than Breast Cancer, HIV, and Motor Vehicle Crashes Combined!
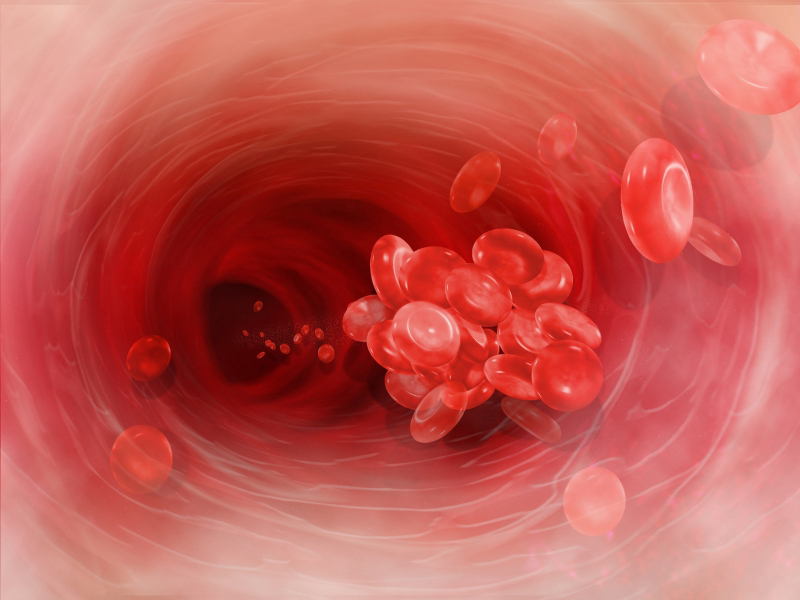
| Red blood cells clumped together form a blood a blood clot (thrombus) that can block blood flow in the body's deep veins, and cause DVT. |
Deep vein thrombosis (DVT) can be a dangerous medical condition caused by the creation of a blood clot (thrombus) in a deep vein of the leg or lower pelvis. Pulmonary embolism (PE) happens when a DVT starts to move through your body and gets stuck in the lungs. This can be life threatening or deadly all of a sudden.
The term venous thromboembolism (VTE), which means a blood clot that starts in a vein, is used to describe both conditions.
DVT can affect people of all ages and backgrounds. Personal risk factors for DVT may change throughout your lifetime depending on your health and events that may change your risk.
It is important to understand your personal risk factors, take steps to prevent DVT, and recognize signs and symptoms if they happen. If you think you may have a DVT, it is very important to seek medical care right away.
Be involved in your care — take steps to prevent DVT blood clots!
The CDC estimates as many as 900,000 people could be affected each year in the United States by a DVT or a PE. It is also suggested that 60,000-100,000 Americans die of a DVT or a PE . This is more deaths than seen from breast cancer, HIV, and motor vehicle crashes combined.
DVT/PE are often underdiagnosed. In fact, 10% to 30% of people will die within one month of diagnosis. Sudden death is the first symptom in about 25% of people who have a PE. It is important to know about DVT/PE because it can happen to anybody at any age, but more in the elderly population.
Half of the people who have ever had a DVT will have long-term complications, such as swelling, pain, discoloration, and scaling in the affected limb. A third of the people with DVT/PE will have a recurrence within 10 years.
The good news: DVT is preventable and treatable if discovered early.
Being hospitalized, obesity, varicose veins, or sitting too long in car rides or plane rides can cause your leg blood flow to slow down and gather in one spot. This is an easy way for a clot to form.
Cancer, pregnancy, taking birth control, hormone replacements and/or smoking make the blood clot easier by making the blood sticky.
Surgery or a big trauma can cause a DVT because the blood vessel is damaged and tries to fix itself with a blood patch.
Download this DVT Risk Assessor to find out your own risk now!
| DVT Pain Tenderness Swelling Warmth Redness | PE Shortness of breath Abnormally rapid breathing Chest pain Rapid heart rate Fainting |
If you have any of the symptoms of a DVT, it is important to seek urgent care from your doctor. To see if you have a DVT, they will do an ultrasound on your leg(s). This is a wand that is moved along your leg(s) to see if you have a DVT.
If you experience any of the symptoms of a pulmonary embolism,
it is an emergency and you should seek medical attention immediately!
To test for a PE, you will need a CAT scan of your chest. A special dye will be put in your vein through an intravenous line (a small catheter in your vein) to take a better picture.
Even if you have risk factors, there are a number of things you can do to decrease your risk. Exercise regularly and maintain a healthy weight. Don't smoke!
If you travel for longer than six (6) hours or are sitting for long periods of time, you should exercise your legs frequently, get up and walk around every two to three hours. Wearing loose-fitting clothing and keeping well hydrated (but staying away from caffeine and alcohol) also can help reduce your risk.
Before and during any hospitalization, talk to your healthcare provider about your risk of blood clots and what can be done to help prevent them. If you have to remain in bed, move around as much as possible and get up when your practitioner says it is okay.
During your hospital stay, you may be given a small dose of an anticoagulant (blood thinner) to help prevent DVT. If a mechanical device such as compression sleeves and pump are ordered, it is important to keep it on at all times except when walking.
| Talk to your doctor about your level of risk! While we sincerely hope you or someone you love never experiences a DVT, it is important to know you have access to advanced treatment and expertise here at Stony Brook University Hospital. Our specially-trained DVT team is an that has reduced the amount of hospital-acquired DVTs. You can also receive outpatient care at our Centereach and Commack locations that specialize in veins for immediate and long-term care. The team is led by Antonios P. Gasparis, MD, professor of surgery and member of our Vascular and Endovascular Surgery Division. |
Posted by Stony Brook Surgery on March 1, 2019
March Is National Colorectal Cancer Awareness Month! Colorectal cancer screening saves lives. If everyone 50 years old or older were screened regularly, as many as 60% of deaths from this cancer could be avoided.
Colorectal cancer — also known as colon cancer — is the second leading cause of cancer-related deaths in the United States. It affects both men and women. Every year, more than 140,000 Americans are diagnosed with colorectal cancer, and more than 50,000 people die from it.
Awareness of colorectal cancer and its common signs is well worth it, because when detected early this cancer can be treated effectively.
Here, Paula I. Denoya, MD, a member of the faculty of our Colon and Rectal Surgery Division, answers frequently asked questions about colorectal cancer, with special attention to its common warning signs, detection, and treatment.
Q: What is colorectal cancer?
A: Colorectal cancer arises from the lining of the colon or rectum, usually from cells that secrete mucus. In many cases, it starts out as a polyp, which is a premalignant, benign lesion or an overgrowth in the lining of the colon. If left alone, a polyp can grow into cancer. However, with screening, polyps can be detected and removed, thus preventing cancer altogether.
Q: What are the signs and symptoms?
A: Colorectal cancer is often symptomless, which is why screening is so important. Some people do experience telltale signs, however. Ten warning signs of colorectal cancer are:
- Blood in stool
- Persistent diarrhea
- Persistent vomiting
- Cramping abdominal pain
- Persistent bloating
- Unexplained weight loss
- Decreased stool size
- Unexplained fatigue
- Change in bowel habits
- Incomplete emptying of bowel
Anyone experiencing these symptoms should speak with their primary care physician.
Q: Who is at risk?
A: According to the American Cancer Society (ACS), colorectal cancer is the third most common cancer in men and women. Gender does not seem to be a factor, but age is, and risk increases after age 50.
People considered to be at higher risk include those with a family history of polyps, colon cancer, or uterine cancer; individuals with inflammatory bowel disease; anyone with a personal history of polyps; and persons with inherited syndromes such as familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer.
The ACS recommends that people undergo screenings starting at age 45. Individuals at high risk should start screenings earlier and have more frequent follow-ups."
Colorectal cancer can be prevented, and it is extremely curable if caught early.
Q: How is colorectal cancer detected?
A: Colonoscopy is considered the gold standard because it is the only test that can identify and treat polyps in the entire colon. Further, if a polyp is detected during screening, it often can be removed and biopsied at that time, eliminating the need for additional procedures. (See our 2012 blog post, "New Report Affirms Lifesaving Role of Colonoscopy: Death Risk Is Cut in Half.")
While people often dread undergoing a colonoscopy, it is important to know that recent changes make it a gentler experience. For example, Stony Brook uses many different kinds of bowel preparations — some are even in pill form. The patient's physician will determine which preparation the patient will best tolerate.
In the past, patients remained awake for the procedure, but now, with innovations in anesthesia, patients undergo a short, fast-working, and deep sedation that has minimal side effects including no memory of the procedure.
Stony Brook offers additional screening methods, including flexible sigmoidoscopy, barium enemas, fecal occult blood testing, and CT colonography, also known as virtual colonoscopy.
Virtual colonoscopy was invented at Stony Brook in the 1980s. While less invasive than a traditional colonoscopy because it uses a CT scan to look at the lining of the colon, it still requires bowel preparation. It is generally used with patients who may have an existing colon blockage or for whom a colonoscopy carries risks, for example, from anesthesia. Unlike a colonoscopy, in which a polyp can be removed during the screening procedure, during a virtual colonoscopy, if a polyp is detected, the patient will need an additional procedure to treat and biopsy it.
Q: If cancer is detected, how is it treated?
A: Colorectal cancers respond well to treatment, and often treatment is relatively uncomplicated. About 30% of cases can be treated with surgery alone. Cancers in later stages respond well to chemotherapy and radiation, and overall, the five-year survival rate approaches 65%.
Colorectal cancer is treatable — know your options.
For patients with colorectal cancer in the lower part of the colon, both the rectum and the anus are often removed. The patient, then, typically needs a permanent colostomy, which collects stool in a bag attached to the belly (abdominal wall).
For some low rectal cancers, Stony Brook's colon and rectal surgeons perform a more advanced type of surgery that eliminates the need for a colostomy and preserves bowel function. Called sphincter-sparing surgery, this procedure allows for removal of the cancer and "spares" the anal sphincter muscle.

Q: What distinguishes Stony Brook's approach?
A: Stony Brook Medicine offers the latest protocols and treatments for colorectal cancers — delivered by a multidisciplinary team — including the new transanal endoscopic microsurgery, a less invasive procedure than the traditional approach for reaching lesions high up in the rectum.
We are renowned leaders in the use of minimally invasive laparoscopic surgery for treating colorectal cancer, which offers patients considerable benefits.
Using the da Vinci® Si robotic surgical system, our surgeons offer patients another option beyond traditional open surgery and laparoscopic procedures. The major advantage of this minimally invasive technique is that it provides surgeons with enhanced visibility and mobility.
This improves accuracy, provides cleaner "margins" (which means that no cancer cells are seen at the outer edge of the tissue that was removed) and helps ensure that all the lymph nodes (difficult to see and reach by conventional methods) can be removed during the procedure.
Benefits to the patient having robotic surgery include less bleeding, less scarring, less pain, and a lowered risk of infection.
In addition, we are working to advance the practice of medicine through clinical trials. We currently offer several clinical trials investigating novel approaches to chemoradiation therapy for rectal cancer and new chemotherapy and immunotherapy options for colorectal cancer.
For standard treatment approaches, we work closely with oncologists, radiologists, pathologists, and other specialists on the colorectal cancer multidisciplinary team at Stony Brook Cancer Center to provide comprehensive cancer care to our patients.
If you are over age 50 and have not yet had a colonoscopy, schedule one soon by calling Stony Brook's Direct Access Screening Colonoscopy Program at 631-444-COLON (2656) . You can request an appointment online, too.
| "Don't Assume" is the Colorectal Cancer Alliance's 2019 National Colorectal Cancer Awareness Month public awareness campaign. Its goal is to challenge assumptions and misconceptions about colorectal cancer by dispelling myths, raising awareness, and connecting people across the country with information and support. Learn more about the campaign. |
Posted by Stony Brook Surgery on February 27, 2019
It's the Final Week of American Heart Month and Time to Gather All the Takeaways
By Joanna Chikwe, MD, Chief, Cardiothoracic Surgery Division, and Director, Heart Institute
February means heart health awareness, but taking care of your heart requires a year-round commitment that has lifelong benefits. What will you do differently to take better care of your heart?
Heart disease can affect anyone, regardless of gender, age or background. That's why all of our cardiac care experts at Stony Brook University Heart Institute remain focused on how to best prevent heart disease and heal the heart.
When you come to Stony Brook Heart Institute, you can depend on quality and expertise for every aspect of your cardiac care — care that exceeds national outcomes. A few examples:
- Our renowned team of interventional cardiologists have long been on the forefront for treating acute myocardial infarction, or heart attack. In fact, we exceed national outcomes and have the best outcomes on Long Island when it comes to bringing lifesaving heart emergency care to heart attack victims, as reported on the Hospital Compare website.
We have the best outcomes on Long Island when it comes to
bringing lifesaving heart emergency care to heart attack victims.
- Our heart surgeons have a high degree of expertise in providing advanced approaches to coronary artery bypass grafting (CABG) — a surgical procedure that uses blood vessels from other areas of your body to restore blood flow to your heart.
- For patients with severe aortic stenosis (narrowing), Stony Brook is a leader in advancing the transcatheter aortic valve replacement (TAVR) procedure and is one of a select number of sites in the U.S. to offer this minimally invasive procedure for patients who are considered high, intermediate or low-risk for open surgery.
Stony Brook has excellent long-term data on patient outcomes with TAVR, and we are a tertiary referral center for evaluation of aortic valve disease.
Our Heart Institute has received a three-star rating — the highest awarded — from The Society of Thoracic Surgeons (STS) for overall patient care and outcomes in isolated CABG surgery.
This distinguished award is in recognition of the isolated CABG procedures we performed from January to December 2017. The STS ratings are regarded as the definitive national reporting system for cardiac surgery (read more).
Our patient outcomes for survival with heart failure are the best
on Long Island and among the best throughout the nation.
- And, for patients with heart failure, a condition where the heart can't pump enough blood to meet the needs of the body, our world-renowned experts at the Heart Failure and Cardiomyopathy Center help patients to restore their quality of life, limit their symptoms and understand their disease.
We are proud that our patient outcomes for survival with heart failure are the best on Long Island and among the best nationally, according to Hospital Compare.
While we hope that you and your family never need acute cardiac services, you can be assured knowing that Long Island's only Chest Pain Center with Primary PCI and Resuscitation is right in your community.
And, if you suspect a heart attack, please remember it's best to call 911. Ambulances are equipped with defibrillators and most are equipped with 12-lead EKGs (electrocardiograms), which means they can transmit results to the hospital while en route. At Stony Brook, we assemble the treatment team and equipment you need before you arrive.
Want to do something today to learn about your heart health? Take a free heart health risk assessment at www.stonybrookmedicine.edu/hearthealth. Seeking a solution to a cardiac problem? Call us at 631-44-HEART (444-3278). We're ready to help.
[Grateful acknowledgment is made to TBR News Media for permission to reproduce Dr. Chikwe's article originally published in its newspapers and online on February 22, 2019.]
Posted by Stony Brook Surgery on February 25, 2019
Today is the first day of National Eating Disorders Awareness Week, so now is a good time to learn more about these abnormal eating behaviors, and how the impact they may have on our health.
In the United States, 20 million women and 10 million men will suffer from an eating disorder at some point in their lives.
Eating disorders are serious, potentially life-threatening illnesses that affect all kinds of people, regardless of gender, ethnicity, size, age, or background. In fact, eating disorders have the highest mortality rate of any mental health concern.
Eating disorders are widely misunderstood illnesses and support options are often inaccessible. As a result, too many people are left feeling helpless, hopeless, and frightened.
BED is more common in women than in men. In the United States, about 3.5% of women (5.6 million) and 2% of men (3.1 million) have it. Here, Genna F. Hymowitz, PhD, assistant professor of psychology, psychiatry, and surgery, and director of the behavioral medicine program, L. Krasner Psychological Center, answers frequently asked questions about BED and obesity. Dr. Hymowitz is a member of the multidisciplinary team of our Bariatric and Metabolic Weight Loss Center. Q: What is BED — binge eating disorder? A: BED is a disorder characterized by episodes of eating an objectively large amount of food in a discrete period of time that are accompanied by loss of control of eating and some or all of the following symptoms:
Individuals with BED experience these episodes at least one time a week for at least three months. Although symptoms typically begin in late childhood, early adolescence (ages 11-13), or in young adulthood (ages 25-26), many individuals do not seek treatment until later in life.
At Stony Brook Medicine, we know how best to treat patients with BED and obesity, in terms of
providing care for the whole patient and staging the different treatment options.
Q: What causes BED?
A: A number of factors contribute to the development and maintenance of BED, including genes, the endocrine system, serotonin levels, early family environment, and dietary behaviors.
Although triggers for binge eating episodes vary from person to person, common triggers for binge eating episodes include excessive hunger and negative emotional states, such as stress, or depression.
Q: Who is affected by BED?
A: BED affects up to 7% of individuals in the United States, and occurs in both men and women.
Q: What are BED's risk factors and the problems associated with it?
A: Many, but not all, individuals with BED experience weight and shape concerns, and compared with the general population, individuals with BED are more likely to experience substance abuse, depressive symptoms, and chronic medical conditions, including irritable bowel syndrome, fibromyalgia, insomnia, and metabolic syndrome.
Q: What are the health consequences of BED?
A: BED is also associated with impaired quality of life, higher risk illnesses, higher risk of death, and increased risk for weight gain and development of obesity.
Q: What is the relationship of BED with obesity?
A: Although up to 70% of individuals with BED also experience obesity, only about 8% of individuals with obesity meet criteria for diagnosis of BED.
Individuals with both BED and obesity are more likely to experience more severe obesity and earlier onset of weight difficulties, and to have a greater likelihood of also having depression, substance abuse, and other psychological disorders, such as anxiety.
Here, we not only look carefully to see the person behind every patient, we also understand that
every patient has both physical and psychological dimensions affecting their health.
Q: What is the treatment for BED?
A: There is strong evidence to support the use of cognitive behavioral therapy (CBT) to treat BED. CBT is a skills-based psychological intervention that addresses the patterns of thoughts, feelings, and behaviors that maintain BED symptoms.
Treatment generally involves weekly one-hour sessions and completion of home practice assignments, including self-monitoring, setting up a regular eating schedule, and practice of cognitive techniques and coping strategies discussed in session.
Self-help versions of CBT and other individual psychological interventions, including interpersonal therapy, may also be helpful to address BED.
Additionally, research suggests that some medications can be beneficial for addressing BED, including some stimulant medications, second-generation antidepressants (SSRIs), anticonvulsant medications, and other medications used to address obesity.
Q: How is weight management approached in individuals with BED?
A: Although pharmacological and psychological interventions can address symptoms of BED, many treatments focused on reduction of BED symptoms do not consistently lead to long-term weight loss.
Although individuals with BED can benefit from lifestyle weight loss interventions and bariatric surgery, it is generally recommended that individuals begin to address disordered eating behaviors prior to engaging in additional weight loss interventions.
Q: What is the benefit of seeking treatment for BED and obesity at the Stony Brook Bariatric and Metabolic Weight Loss Center?
A: The benefit is the multidisciplinary care provided at our weight loss center. Here, we not only look carefully to see the person behind every patient, we also understand that every patient has both physical and psychological dimensions affecting their health.
And so, we know how best to treat patients with BED and obesity, in terms of providing care for the whole patient and staging the different treatment options, with emphasis on behavioral transformation.
Posted by Stony Brook Surgery on February 22, 2019
Providing New Therapy to Reduce Disease Severity and Improve Quality of Life

Most people are unaware of deep venous thrombosis (DVT) and its possible consequences. DVT is a blood clot in a deep vein, usually in the legs. It is one of the leading causes of death in the United States.
These blood clots can be dangerous if they break off and travel to the lungs. When this happens, it causes a serious, potentially life-threatening condition called pulmonary embolism (PE).
The precise number of people affected by DVT/PE is unknown, although as many as 900,000 people could be affected (1 to 2 per 1,000) each year in the United States, according to the Centers for Disease Control and Prevention.
PE is the most serious complication of DVT. In addition, nearly one-third of people who have a DVT will have long-term complications caused by the damage the clot does to the valves in the vein. This condition is called post-thrombotic syndrome (PTS).
There is broad consensus that C-TRACT addresses a health question of major importance
to patients, physicians, and the U.S. healthcare system.
PTS is a common long-term complication of lower extremity DVT, and often causes pain, swelling, and skin changes (sometimes including venous wounds) in the affected limb. In some cases, the symptoms can be so severe that a person becomes disabled.

The Chronic Venous Thrombosis: Relief with Adjunctive Catheter-Directed Therapy (C-TRACT) clinical trial is a multicenter, randomized controlled clinical trial designed to determine if the use of image-guided, endovascular therapy is an effective strategy to reduce PTS disease severity and to improve quality of life in patients with established disabling PTS.
In this study, all patients will receive high-quality standard PTS care, and approximately 50% of patients will be randomly assigned to receive endovascular therapy, which consists of stent placement for iliac vein obstruction in the legs.
Patients will be followed for two years. The main outcomes assessed will be the degree of improvement in PTS severity, quality of life, venous ulcer healing, safety, and cost-effectiveness.
Antonios P. Gasparis, MD, professor of surgery (Vascular and Endovascular Surgery Division) and director of the Center for Vein Care and the Non-Invasive Vascular Lab, is leading the participation of Stony Brook Medicine in this study.
The study is funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health and led by the Washington University School of Medicine.
The need for the C-TRACT trial has been endorsed by multidisciplinary organizations including the American College of Phlebology, American Venous Forum, North American Thrombosis Forum, Society of Interventional Radiology Foundation, and Society for Vascular Medicine. There is broad consensus that C-TRACT addresses a health question of major importance to patients, physicians, and the U.S. healthcare system.
| Attention physicians: C-TRACT plans to enroll 374 subjects at 20-40 clinical centers. To reach this enrollment goal, the C-TRACT Referral Tool App was designed to securely connect physicians who have potential study candidates to participating sites and can be downloaded to a mobile device. Providers are encouraged to download the C-TRACT Referral App. |
Posted by Stony Brook Surgery on February 18, 2019
Stony Brook University Heart Institute Provides Transcultural Care for Spanish-Speaking Patients
By Jorge M. Balaguer, MD, of Our Cardiothoracic Surgery Division & the Heart Institute
More than 53 million Hispanics live currently in the United States. They constitute 17% of the total U.S. population, and represent the fastest-growing ethnic population. Hispanics are expected to represent 30% of the total U.S. population by 2050 (132 million people).
Mexican, Puerto Rican, and Cuban are the most common Hispanic groups; however, Colombian, Dominican, Guatemalan, and Salvadorian populations have been increasing at an accelerated rate in the last decade.
On Long Island, the Hispanic population exceeds 500,000 people. In the southern districts of the Island, the Hispanic population is more prevalent.
Cardiovascular disease (CVD) involving the circulatory (blood) system is the highest cause of death among Hispanics, as it is for the rest of the population of the United States. The incidence of certain forms of CVD is documented to be higher among Hispanics.
Coronary artery disease (CAD) — the obstruction of arteries that provide blood supply to the heart muscle leading to heart attacks, heart failure, and sudden death — is higher in some Hispanic groups.
The rate of CAD based upon imaging diagnostic studies shows there is a significant difference between patients with and without risk factors.
Risk factors for cardiovascular disease are more prevalent among Hispanics/Latinos
in the United States and on Long Island than in the general population.
The prevalence of CAD among Hispanics older than 40 years was 10% if they did not have risk factors versus 70% if they have high cholesterol, have diabetes, and were smokers.
One study conducted in Mexicans older than 65 years showed that the rate of heart attacks is much higher than in non-Hispanics and particularly higher in Mexican women.
The rate of heart attacks in Hispanics is 7.2% in patients older than 65 and 12% in older than 75 years.
The rate of ischemic stroke (brain attack) as well as the prevalence of stroke at an early age is higher among Hispanics compared to non-Hispanic whites. Mexicans are at a higher risk to develop hemorrhagic stroke (aneurysm burst or weakened blood vessel leak in brain) compared to other populations.
The incidence of heart failure in Hispanics is higher compared to non-Hispanic whites. Among Medicare enrollees, hospitalization for heart failure is higher among Hispanics.
Heart failure is more prevalent among Hispanic men than women. Hispanics with heart failure were more likely to be younger, to have diabetes or high blood pressure, and to be overweight or obese.
The modification of risk factors associated with CVD is critical to minimizing the impact of CVD and stroke in the general population.
Risk factors in the Hispanic population show some differences compared to non-Hispanic populations which are detailed as follows:
According to a recent study, almost 50% of Mexican men and women older than 20 years have a total cholesterol level greater than 200 mg/dL which is considered high.
Almost 40% have a LDL cholesterol level (bad cholesterol) greater than 130 mg/dL which is also considered high, increasing the risk of developing CVD.
Among Hispanic men, Mexicans have the highest incidence of high cholesterol.
Among Hispanic women, Puerto Ricans showed the highest levels of LDL cholesterol.
Despite this high incidence of risk factors, only a small percentage of Hispanic men and women get screened, or are aware of their cholesterol levels.
Despite the high incidence of risk factors, only a small percentage of Hispanic men
and women get screened, or are aware of their cholesterol levels.
Cholesterol goals, according to the American Heart Association, are:
- Total cholesterol less than 200 mg/dL
- LDL cholesterol (bad cholesterol) less than 100 mg/dL
- HDL cholesterol (good cholesterol) greater than 60 mg/dL (slightly lower levels accepted)
Approximately 30% of Hispanics — both males and females — have high blood pressure (hypertension).
Hispanic individuals remain more likely to have undiagnosed, untreated, or uncontrolled hypertension. Some studies have shown a much higher incidence of hypertension compared to non-Hispanic whites.
Puerto Rican Americans have the highest rate of mortality associated with high blood pressure. Cuban Americans and Hispanic women from South America appear to have the lower rates of high blood pressure.
The goals for blood pressure are less than 120 mm/Hg systolic (the pressure when the heart contracts) and less than 80 mm/Hg diastolic (the pressure when the heart relaxes between beats), according to the American Heart Association.
Type 2 diabetes is highly prevalent among Hispanics. It is twice as high compared to non-Hispanics.
The chance of Hispanics dying from conditions associated to diabetes is 50% higher than in other populations.
Mexicans and Puerto Ricans appear to have a higher incidence of diabetes. Young Hispanic and Hispanic children of Mexican descent are also at a higher risk of diabetes.
Not only is the incidence of diabetes higher in Hispanics, but the blood sugar levels also do not seem to be well controlled among them. This leads to kidney and visual problems over time.
The language barrier between Hispanic patients and healthcare providers and limited access to healthcare are postulated as responsible for these findings.
The goal of blood sugar before meals should be 100 to 130 mg/dL, according to the American Diabetes Association.
Overall, the prevalence of cigarette smoking in Hispanics is lower than other populations, and has shown a significant decline during the last decades. Smoking prevalence was lower for women (15%).
There is a wide variation among different Hispanic groups. Mexican and Cuban men and Puerto Rican women are the groups with a higher prevalence of smoking.
Obesity is highly prevalent among Hispanics. Some studies show that more than 70% of males and females in some Hispanic groups are overweight (body mass index greater than 25) and 30% to 40% are obese (body mass index greater than 30). Obesity is higher in Hispanic women.
During the last few decades, obesity has been increasing among Hispanics.
Obesity contributes to other risk factors for CVD, including diabetes, high blood pressure, and high cholesterol. It is also associated to pulmonary issues, joint stress and other medical conditions.
Activity
Several studies have shown that Hispanics are the most physically inactive ethnic group in the United States when considering leisure exercise. Older Hispanic women seem to be the least active group.
On the other hand, a high percentage of Hispanics have physically active jobs which might balance the lack of activity during leisure time.
Combined Risk Factors
Only 20% of Hispanic men and 30 % of Hispanic women are considered to be in the low-risk category for CVD based upon risk factors.
Puerto Ricans seem the Hispanic group with the higher association of all major CVD risk factors (high cholesterol and blood pressure, diabetes, obesity, and smoking).
When looking at the association of three major risk factors, the prevalence among Hispanic men is around 20%, higher than among Hispanic women (17%).
It seems that U.S.-born Mexicans have a higher risk factors profile than Mexicans and non-Hispanic whites.
Language is often a barrier faced by Hispanic patients in accessing healthcare.

Although the use of interpreter services is helpful, the communication via interpreters is often lengthy and indirect. When patients' family members serve as interpreters, they might interfere with the content of the communication despite their best interests.
The ideal situation is when providers and patients communicate in the same language at a high level of competency.
When Hispanic patients have limited command of the English language, the risk of incomplete or inaccurate communication is high.
When healthcare providers are fluent in Spanish and demonstrate cultural understanding of the Hispanic culture, an ideal communication and emotional connection between patients and providers is established, fostering trust and empathy.
At Stony Brook Medicine, there is a high level of awareness of ethnic and cultural differences of Hispanic populations.
In order to lessen the emotional burden of the language barrier, Hispanic patients have the option to contact the Stony Brook Heart Institute in their preferred language.
En el Instituto del Corazón de Stony Brook hablamos español: Jorge M. Balaguer, MD, cardiothoracic surgery, Stony Brook University Hospital — Elliott Bennett-Guerrero, MD, anesthesiology and critical care, Stony Brook University Hospital — Mai-Ling Colon, staff assistant, cardiothoracic surgery, Stony Brook University Hospital — Anthony Escano, RN, critical care (cardiothoracic intensive care unit [CTICU]), Stony Brook University Hospital — Fabiola Garcia, RN, critical care (CTICU), Stony Brook University Hospital — Monica Fox, RN, heart failure cardiology, Stony Brook University Hospital — Lucia Joya, administrative assistant, cardiothoracic surgery, Stony Brook University Hospital — Jennifer Rojas, office manager, cardiology, Stony Brook Southampton Hospital.
Stent implants (angioplasty, also called percutaneous coronary intervention), coronary bypass graft surgery (CABG), and hybrid revascularization (combination of stent placement and bypass surgery) are the most common modalities in advanced treatment of CVD.
Stents have shown to be a superior treatment for some heart attacks and for less severe forms of CVD.
CABG is the preferred treatment for the severe forms of CVD.
The cardiac surgery team at Stony Brook has been awarded a three-star rating by the Society of Thoracic Surgeons for its outstanding performance with CABG surgery compared to all other programs in the United States (read more).
The goals established by the American Heart Association — to improve by 2020 the cardiovascular health of all Americans by 20%, while reducing deaths from cardiovascular diseases and stroke by 20% — are fully endorsed by Stony Brook Medicine.
The Stony Brook Heart Institute is committed to fighting CVD at all levels: prevention, early diagnosis, and treatment.
Our heart team of cardiologists and cardiac surgeons is fully equipped with the state-of-the-art techniques, technology, and expertise to deliver superior care.
| Summary: Risk factors for cardiovascular disease (CVD) are more prevalent among Hispanics/Latinos in the United States and on Long Island than in the general population. These risk factors are associated with the development of coronary artery disease (cholesterol plaques built up inside the arteries in the heart causing blockages) leading to heart attacks, heart failure, stroke mortality, and disability. Most of these risk factors can be modified with medications, diet, and life-style changes leading to a decreased incidence of CVD. Early diagnosis and treatment with state-of-the-art techniques and technology are available at the Stony Brook Heart Institute. We have Spanish-speaking providers and access staff (tenemos los proveedores de salud y las personas de acceso que hablan español). |
|
|
Posted by Stony Brook Surgery on February 15, 2019
We are very pleased to announce the publication of Clinical Algorithms in General Surgery: A Practical Guide, co-edited by Salvatore Docimo Jr., DO, MS, assistant professor of surgery, and a member of our Bariatric, Foregut, and Advanced Gastrointestinal Surgery Division, and Eric M. Pauli, MD, associate professor of surgery, of Pennsylvania State University.
Published by prestigious international science publisher Springer, this 873-page text comprising 43 chapters takes the major pathologies of the systems commonly studied in general surgery and presents them in a unique format based upon algorithms.
The algorithms begin with the clinical presentation of the patient, work their way through the various diagnostic modalities available to the surgeon, and finally allow the physician to make a decision regarding treatment options based upon various patterns in the algorithms.
As the field of general surgery continues to expand, the diagnostic and therapeutic pathways are becoming more complex.
Numerous authors who contributed to the text are faculty and residents of our Department of Surgery.
"This is a practical handbook that will be an excellent guide for learners at all levels in surgical practice," says Aurora D. Pryor, MD, professor of surgery and vice chair for clinical affairs, and chief of the Bariatric, Foregut, and Advanced Gastrointestinal Surgery Division. "I think it will be a well-used resource for patient care."
The diagnostic modalities available to the clinician can be both very helpful but also overwhelming considering the findings can often determine the scope of treatment for a patient.
Clinical Algorithms in General Surgery is designed to be a very useful resource for surgeons as it allows complex clinical pathways to be conveniently organized in logical algorithms.
This text is a concise yet comprehensive manual to assist in clinical decision-making. All algorithms have been reviewed by experts in their field and include the most up-to-date clinical and evidence-based information.
Numerous authors who contributed to the text are faculty and residents in our Department of Surgery: faculty, Andrew T. Bates, MD, Joanna Chikwe, MD, Lukasz Czerwonka, MD, Georgios V. Georgakis, MD, PhD, Samer Sbayi, MD, Konstantinos Spaniolas, MD, and Henry J. Tannous, MD; residents, Maria S. Altieri, MD ('18), Ewen Chao, MD (PGY-2), Carl J. Dickler, MD (PGY-5), Jessica C. Gooch, MD ('17), Anish Shah, MD (PGY-4), and Michael G. Svestka, MD ('18). Several of these authors provided multiple chapters.
Clinical Algorithms in General Surgery provides a useful resource for surgeons in clinical practice as well as surgical residents, and surgical attendings who are preparing for board examinations.
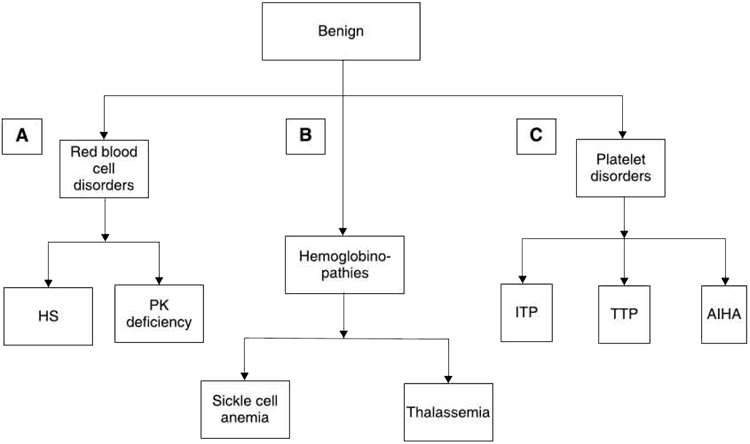
Atraumatic Indications for Splenectomy: Benign Conditions
Posted by Stony Brook Surgery on February 13, 2019
Dedicated to Helping Communities Here and Abroad since Joining Our Faculty
We are very pleased — and proud — to share the news that Richard J. Scriven, MD, associate professor of surgery and pediatrics, is the winner of the 16th annual Michael A. Maffetone Community Service Award for his "tireless work in communities in need here and in Africa, Ecuador, and Puerto Rico."
Board certified in both general surgery and pediatric surgery, Dr. Scriven is a member of our Pediatric Surgery Division, and also serves as the pediatric trauma medical director and the program director of the general surgery residency program.
The Maffetone Award recognizes a current employee of Stony Brook Medicine or the Long Island State Veterans Home who demonstrates outstanding community service in education, healthcare, human services, arts and culture, diversity, safety, or injury prevention.
Preference is given to activities directed at eliminating disparities in access to quality healthcare. Partisan political activities, sectarian religious activities, or service that is part of the nominee's normal job responsibilities are excluded from consideration. The individual chosen for this honor is recognized with a $1,000 award.
"Tireless work in communities in need here and in Africa, Ecuador, and Puerto Rico"
Dr. Scriven has a long history of community service outside his normal job responsibilities ever since joining our faculty in 2001. Upon his arrival he joined the Stony Brook Fire Department as a volunteer firefighter, doing work details and fighting fires. He currently serves as the fire department's medical director and on its board of directors.

| Dr. Scriven (right) with fellow members of the Stony Brook Fire Department in 2014, following emergency delivery of twin premature infants in the mother's house; the story was featured on CBS New York News (click on image to enlarge). |
Dr. Scriven has served for several years as a board member of Blanca's House, the Long Island-based organization of volunteer healthcare professionals who provide free medical treatment to people without access to good healthcare, largely in Latin America.
Blanca's House has coordinated numerous medical missions to Ecuador, with Dr. Scriven on many of them. There, he has provided care for patients of all ages who require general surgery procedures, often hernia repairs and gallbladder removals.
In 2011, Dr. Scriven went on a medical mission to Africa with colleagues in the Department of Pediatrics to help children there.
Dr. Scriven was recognized by the Village Times Herald newspaper as the 2006 Man of the Year in Medicine for his dedication to his patients and for his contributions to the local Three Village community.
In 2016, he received the service award from Blanca's House for “support, commitment, and dedication to the vision and mission of Blanca's House" (i.e., medical missions in Latin America).

| Dr. Scriven (right) with operating room teammates on their five-day Blanca's House medical mission in 2018 in Santa Elena, Ecuador, where he provided pro bono surgery for the underserved community (click image to enlarge). |
In 2017, he received the Leonard Tow Humanism in Medicine Award for demonstrating “both clinical excellence and outstanding compassion in the delivery of care" and showing “respect for patients, their families, and healthcare colleagues."
Soon after Hurricane Maria devastated the Caribbean islands, in 2017, Dr. Scriven took part in Stony Brook Medicine's 16-day medical mission in Puerto Rico, which was crippled by the hurricane.
Dr. Scriven, who was one of three physicians from Stony Brook on the mission, contributed his expertise as a pediatric trauma specialist (read more).
Together, Dr. Scriven's nearly two decades of multi-faceted activity helping communities here and abroad, since joining our faculty, clearly justify his winning this year's Maffetone Award.
Dr. Scriven received his MD in 1990 from the Albert Einstein College of Medicine, and then completed his training in general surgery and pediatric surgery at the SUNY Health Science Center at Brooklyn.
Recognized as a top pediatric surgery specialist, Dr. Scriven has been selected for inclusion on New York Magazine's “Best Doctors" list, representing the top 2% of physicians in the greater New York metropolitan area, and also selected for inclusion in the Castle Connolly Guide, Top Doctors: New York Metro Area.

Dr. Scriven was nominated for the Maffetone Award by Christopher S. Muratore, MD, chief of pediatric surgery; Helen Hsieh, MD, PhD, and Michelle L. Ceo, CPNP, Pediatric Surgery Division; Eric Niegelberg, NREMT-P, MS, Christine Nastasi, RN, and Erin A. Zazzera, RN, MPH, Trauma, Emergency Surgery, and Surgical Critical Care Division; Alexander B. Dagum, MD, chief of plastic and reconstructive surgery and board member, Blanca's House; Elizabeth Markey, Emergency Department; and Denis Lynch, Stony Brook Fire Department, and past commodore, Stony Brook Yacht Club, where Dr. Scriven is an officer and serves as fleet surgeon.
Michael A. Maffetone, DA, served as director and chief executive officer of Stony Brook University Hospital from 1994 to 2000. Dr. Maffetone was deeply committed to community service, especially for the underprivileged and underserved, and was instrumental in expanding the hospital's community service programs.
Among his many achievements were helping to develop the annual Walk for Beauty, a community event to raise funds to benefit patients with cancer and to support cancer research; opening a magnetic resonance imaging center; planning the Ambulatory Surgery Center; and establishing the relationship that led to the opening of the Carol M. Baldwin Breast Care Center in 1997.
Dr. Maffetone passed away in 2003 at the age of 52. To honor his memory and legacy, Stony Brook University Hospital instituted the annual Michael A. Maffetone Community Service Awards, one for an individual and one for an organization.
| The four-fold mission of Stony Brook Medicine — as originally mandated in the late 1960s by New York State's Department of Health for our Health Sciences Center (HSC) — is patient care, education, research, and community service. At that time University Hospital, then planned and eventually opened in 1980, was an integral part of the HSC. Thus, community service in relation to patient care and population health has long been central to what we are all about here at Stony Brook. |
Posted by Stony Brook Surgery on February 8, 2019
Time to Learn about Common Problems Children Have in the Ear, Nose, and Throat

While children can be affected by ear infections, tonsillitis, or sinusitis, or other ailments of the ear, nose, and throat at any time, they can be especially frequent during February and the other coldest months of the year.
Tonsillectomy with or without adenoidectomy is one of the most common procedures performed in children, with over 470,000 done every year.
This number has declined since the 1970s, when it peaked at 1.5 million tonsillectomies in a year. At that time, 90% of tonsillectomies were performed for recurrent infections. However, now 20% of tonsillectomies are performed for infections, and 80% are performed for obstructive sleep apnea (OSA).
Tonsillitis is an infection of the tonsils, which may be caused by a virus such as the common cold, or a bacterial infection, such as streptococcus (strep throat).
The pharyngeal tonsils are found in the throat and can often be seen as two round masses in the back of either side of the mouth. Adenoids are at the back of the nose and above the roof of the mouth or palate, and cannot be seen through the mouth or nose without special instruments.
There are also lingual tonsils found at the very back and deepest part of the tongue. The tonsils and adenoids are a part of the immune system called lymphoid tissue. They help produce antibodies to fight infections in the body.
If the tonsils are affected by a virus, no medicines are needed, and children should get better after 7-10 days.
Strep throat infections caused by the bacteria Streptococcus pyogenes can be treated with antibiotics.
Children with strep throat often have a high fever, swollen lymph nodes in the neck, or pus on the tonsils. They may also complain of throat pain, or stomach pain, fatigue, or difficulty eating and drinking.
Some infections can also develop into an abscess, or if untreated streptococcal infections can lead to problems with the kidneys or the heart.
If your child has a sore throat, most pediatricians' offices can perform a rapid strep test and/or a throat culture to confirm if there is a streptococcus infection by swabbing your child's throat.
If your child has frequent recurrent episodes of tonsillitis, they may benefit from tonsillectomy.
When children have tonsillitis, the swelling of the tonsils and adenoids can often obstruct the airway when sleeping. Some children also have adenoids and tonsils that are large enough to obstruct the airway without infection.
Signs of enlarged adenoids may include breathing through the mouth instead of the nose, nasal congestion, a muffled voice, or noisy breathing during the day. Enlarged tonsils may cause difficulty swallowing.
If your child snores, or gasps for air or stops breathing at night, they may have sleep apnea.
Sleep apnea is as common as 1-4% in otherwise healthy school-age children. Because of the frequent disturbance in their sleep, they may be very tired during the day, have problems with their concentration and difficulty with performance in school, or have problems with bed-wetting.
If your child has sleep apnea, or OSA, taking out the tonsils and/or adenoids may help with these behaviors.
The gold standard for the diagnosis of OSA is called a sleep study (technical term is polysomnogram). During a sleep study, your child would spend the night at a testing center with monitors while they sleep. These monitors record brain waves, oxygen level in blood, heart rate and breathing, as well as eye and leg movements.
However, not all children may need a sleep study to diagnose OSA. Experienced ENT specialists like our team at Stony Brook Medicine can help to evaluate your child if you suspect he or she may have sleep apnea.
|
To prevent the spread of germs that cause infections and keep your kids healthy this winter season, teach your child to:
|
Posted by Stony Brook Surgery on February 4, 2019
Women Need to Be Proactive in the Prevention and Treatment of Vascular Disease
By Angela A. Kokkosis, MD, Director of Women's Vascular Health, Vascular and Endovascular Surgery Division
Great strides have been made in recognizing cardiac disease in women, but we still lag in the diagnosis and treatment of vascular disease in women.
Vascular disease, which affects the blood vessel's of the entire body, is another aspect in women's health that is not completely understood, resulting in erroneous and/or late diagnosis.
It is vital for women to be aware of their own risk factors, signs, and symptoms, so they can be proactive in the prevention and treatment of vascular disease.
We do know that women over the age of 60 are at increased risk of developing abdominal aortic aneurysms (AAAs), carotid (neck) artery disease, and peripheral artery disease (PAD).
By age 70, this risk is the same as it is for men, and it is believed that women "catch up" to men once they are in menopause and lose the protective effects of estrogen in the cardiovascular system.
As with heart disease, women with certain vascular conditions may have different signs and symptoms than men, which can result in delays in diagnosis and potentially worse outcomes.
Women need to be aware of their own risk factors, signs, and symptoms,
so they can be proactive in the prevention and treatment of vascular disease.
For example, women may be misdiagnosed with arthritis or spinal stenosis, as this is assumed to be more common in women, but they may actually have PAD.
Abdominal aortic aneurysm. The aorta is the main blood vessel in the body which supplies vital nutrients and oxygen to all the major organs. Risk factors such as cigarette smoking, high blood pressure, high cholesterol, and family history can predispose certain women as well as men to develop aneurysms, or a "ballooning," in the aorta.
Typically, the aneurysm develops in the aorta that is in the abdominal region, but it may also occur in the chest (thoracic aortic aneurysm).
Lack of recognition of an aneurysm may put the patient at risk of life-threatening rupture of the aorta.
Unfortunately, aneurysmal disease is a "silent" disease — there are no early symptoms, only the symptoms of rupture (severe, sudden-onset belly pain and/or back pain).
The good news is that a simple non-invasive test, an ultrasound, can effectively diagnose the presence of an abdominal aortic aneurysm. Once an aneurysm is found, a treatment plan can be developed with the patient to determine whether medical management, open surgery, or a minimally invasive "endovascular" (through inside the vessels) repair surgery is indicated.
Carotid artery disease. The carotid artery in the neck serves as one of the main suppliers of blood to the brain; and there is one for each side of the brain. If this artery becomes blocked (typically with atherosclerosis), the patient may be at risk for a serious stroke.
Risk factors for developing these blockages include high cholesterol, cigarette smoking, diabetes mellitus, high blood pressure, and family history.
Early diagnosis of carotid disease is paramount because studies have shown that medical management can effectively delay the progression of carotid disease, and ultimately the risk of stroke.
The types of medications used include those that control high blood pressure, those that help block the "stickiness" of platelets in the blood (antiplatelets), and those that help reduce cholesterol (statins).
If the blockage is very severe, then surgery may be necessary to prevent stroke, and depending on the individual patient, there are both open surgical (carotid endarterectomy) and minimally invasive surgical options (TCAR and carotid artery stenting).
Early diagnosis is certainly feasible; with a simple ultrasound, carotid disease can be discovered, and based on the severity, a treatment plan can be immediately initiated. This is particularly important as carotid disease is another "silent" disease — the first symptom may be the unfortunate stroke!
Peripheral artery disease. The "peripheral" arteries typically describe the arteries in the arms and legs. However, it is the legs which are most affected by vascular disease.
PAD is the build-up of atherosclerosis in the arteries, which leads to blockages. The risk factors for PAD are the same as for carotid disease and heart disease: high cholesterol, high blood pressure, cigarette smoking, diabetes, and family history.
If the blockages are severe enough, the patient may begin to develop early signs and symptoms which include: calf or thigh muscle cramping with walking, hair loss below the knees, abnormal nail growth, or slow healing of minor cuts and scrapes.
As the blockages progress, the patient may notice that it is hard to walk at all because of severe pain on the top of their feet, or they may have already developed wounds or gangrene. In these later stages of PAD, without medical or surgical care the patient is at risk for limb loss.
Early diagnosis is key, as emphasized above. Medical management and exercise therapy can help delay both the need for surgical interventions and reduce the risk for limb loss. However, in the more advanced stages of PAD, there are a myriad of open and minimally invasive endovascular surgical options for patients.
If a patient has the risk factors for PAD or any of the signs and symptoms, a non-invasive test called an "ABI" (ankle brachial index test) can be done to diagnose PAD. Briefly, a blood pressure cuff is placed around the ankles and the upper arms, and the ratio of the blood pressures determines the presence and severity of PAD.
Better understanding of the gender differences in vascular disease with focused randomized trials, biomedical research, and identification of gender-specific medical and social risk factors will improve the clinical outcomes in women.
It is critical for every woman to understand her individual risk of developing vascular disease and, when a vascular condition is diagnosed, to have it managed by a team of experts that can effectively prevent disease progression and complications.
| As a national leader in the diagnosis, treatment, and prevention of vascular disease, the Stony Brook Vascular Center has established clinical and educational programs, both out in the local community and at our Centereach center location, aimed at improving women's vascular health. From meditation to smoking cessation to vascular awareness classes. Free vascular disease screenings are offered throughout Suffolk County to help grow awareness of the need for women to care for their vascular health. |
See information about our FREE vascular disease screenings. Early diagnosis is best for lifesaving treatment. DON'T DELAY — MAKE AN APPOINTMENT TODAY!
Posted by Stony Brook Surgery on February 1, 2019
Today Is National Wear Red Day in Support of Women's Heart Health and the Uniqueness of a Woman's Heart
By Allison J. McLarty, MD, of Our Cardiothoracic Surgery Division & the Women's Heart Center
Today is the first day of American Heart Month and the "Wear Red Day" for promoting women's heart health. Now is a good time for women as well as men to learn about heart disease in women.
Here's the dilemma: Fifty percent of women experience atypical symptoms of "ischemic" heart disease, which is caused by inadequate blood supply (circulation) bringing oxygen to the heart.
The potentially deadly problem is due to blockage in the heart's arteries. That's why it's called ischemic. This medical term means decrease in blood supply. The coronary arteries feed the heart oxygen that it needs to keep working — to keep us alive.
The unfortunate reality is, fewer women than men with ischemic heart disease are referred for diagnostic testing or therapeutic intervention such as angioplasty (stenting) or bypass surgery. And even after such intervention, the outcomes for women are worse than that of men.
Why does it matter so much? Because heart disease is the number one killer of men and women in the United States.
Almost half a million American women have heart attacks each year. Of those, 42% of them die within one year. So about 250,000 women in this country die from heart attacks each year, six times as many as from breast cancer!
This counts as a national crisis which is why the American Heart Association (AHA) and the Centers for Disease Control and Prevention (CDC) over the last decade have made women's heart health a priority with national programs to educate women, as well as their health providers and families, about the unique nature of a woman's heart.
A great example is the Go Red for Women campaign by the AHA which we celebrate in the month of February.
The Go Red for Women campaign is designed to serve as a catalyst for change to improve the lives of women.
It used to be thought in the 1970s that ischemic heart disease (also known as coronary artery disease) was a man's disease only, like prostate cancer. This was in part because most women develop ischemic heart disease a decade or two later in life, after menopause, when the protective effect of naturally produced estrogen is lost.
Women, therefore, tend to be older with more co-existing medical problems like hypertension, diabetes, and obesity attending their heart disease, compared to men.
Additionally, in early clinical trials of stress testing as diagnostic for ischemic heart disease, women presenting with both signs/symptoms of reduced blood flow and positive stress test had normal coronary arteries seen on angiogram — leading to the conclusion that stress testing was "unreliable" in women, coronary artery disease was uncommon in women and symptoms were from other sources, often labelled "stress" or "anxiety."
The problem was that as treatment for heart disease improved over the next few decades and the cardiovascular death rate decreased, it did not do so for women. Finally, medicine "wised" up and the important WISE trial (Women's Ischemia Syndrome Evaluation) was performed in the early 2000s.
| Heart showing coronary arteries; note twig-like branches coming off main trunks (click on image to enlarge). |
To understand ischemic heart disease and the importance of this study, it's important to understand that the heart is a muscle and needs blood to bring it oxygen like any other muscle in the body.
The arteries feeding the heart muscle are known as coronary arteries. These arteries branch, like the branches of a tree, ending in little "twigs" known as capillaries. The larger arteries sit on the surface of the heart, and these are seen on angiograms and treated with angioplasty with stents or bypass surgery in the event of significant blockages. This has long been the principal way to diagnose and treat coronary artery disease.
The WISE trial showed for the first time the importance of the smaller vessels — the "microvascular coronary arteries" — which had been mostly ignored. These tiny blood vessels can spasm or inadequately relax, and cause significant obstruction to blood flow to the tissues of the heart, thus causing chest pain or heart attacks.
And wouldn't you know it, this form of heart disease is more common in women than men. Which helps explain the difference in symptoms, testing results, and treatment results in many women compared to men.
Unfortunately, optimal treatment for this form of ischemic heart disease is still poorly understood. The mainstay of therapy includes currently available medicines for heart disease and a strong push for risk reduction.
So, how should women and those who care about them best care for their hearts?
Aging and family history of early heart disease are risk factors that we cannot change. But other traditional risk factors such as cigarette smoking, uncontrolled hypertension, uncontrolled diabetes, elevated cholesterol, obesity, and a sedentary lifestyle are very much in our hands.
We have power to make changes — to reduce risk factors — that will impact the incidence and course of heart disease and save our lives.
Armed with this knowledge, it behooves us to take control of our health and ensure that we are proactive in decreasing our individual risk of heart disease.
We have power to reduce risk factors that will impact the incidence and course of heart disease and save our lives.
It is also important to be aware of the impact of emerging non-traditional risk factors that we are beginning to understand, such as the inflammation of certain autoimmune disease, hypertensive disorders of pregnancy, gestational diabetes, and depression.
And finally, women should be aware of the symptoms, both classic and atypical, that might herald ischemic heart disease.
Thus, traditional symptoms include chest pain/pressure radiating up the left jaw and down the left arm, intense nausea, dizziness, associated cold sweat.
Atypical symptoms might include persistent heartburn, back pain, atypical chest pain, fatigue/weakness, or palpitations.
Seeking timely medical advice, and discussing the full spectrum of ischemic heart disease with their heart doctor, including the role of both epicardial and microvascular coronary disease, will allow women to be partners in their own heart health and their own greatest advocate.
| The Women's Heart Center of the Stony Brook Heart Institute offers a comprehensive approach to addressing gender-based differences in cardiac health and heart disease through treatment, education, and research designed specifically for women. Our university-based center is the first of its kind in the Long Island and New York City area. We provide a wide range of services especially for women. We focus on risk assessment, evaluation, and risk management. Plus, a full range of care for the hearts of women. |
Learn more about what's good for everyone's heart from the CDC. See Stony Brook Heart Institute's FAQs about women's heart matters. For consultations with our heart specialists, please call 631-44-HEART (444-3278).
Posted by Stony Brook Surgery on January 21, 2019
He Lived and Breathed Our Department and Medical Center until the End

Pediatric surgeon Cedric J. Priebe Jr., MD, professor emeritus of surgery, passed away on Saturday, January 19, at the age of 88 (three weeks shy of his 89th birthday). The founder of our Pediatric Surgery Division, Dr. Priebe had dedicated himself to the advancement of the surgical care of children and the Department of Surgery for nearly four decades.
Dr. Priebe joined our faculty in 1982 as professor of surgery and chief of pediatric surgery. In 2007, after 25 years of distinguished service at Stony Brook, he retired from our full-time faculty.
However, not wanting to quit entirely, Dr. Priebe continued to serve on a part-time basis, contributing to our quality assurance initiatives and also to our educational programs. Right up to very recently, he would routinely attend our weekly pediatric surgical conference.
Dr. Priebe began his distinguished career as an academic pediatric surgeon during the period when the specialty of pediatric surgery was originally developed, in the decades following the Second World War.
Dr. Priebe's sustained desire to constantly improve the surgical care of children was the dominant force guiding his life.
He received his MD in 1955 from Cornell Medical College, and went on to complete his general surgical residency at Roosevelt Hospital in New York City (treats guy in ER that Mickey Mantle punched). He then served in the United States Air Force as a general surgeon for five years.
After caring for a number of complicated pediatric surgical patients, he was stimulated to enter a two-year fellowship in pediatric surgery at Ohio State University's Columbus Children's Hospital under the direction of H. William Clatworthy Jr., MD, that ended in 1967.
Following this training in pediatric surgery, Dr. Priebe returned to practice at Roosevelt Hospital and serve on the faculty at Columbia University. There he developed an academic career and rose to be an associate professor of surgery.
After 12 years he then became a full professor and chief of pediatric surgery at Louisiana State Medical Center and Charity Hospital and director of surgical education at Children's Hospital in New Orleans.
In 1982, when Stony Brook University Hospital was new, and the Department of Surgery was transforming from a group of "generalists" into groups with more specialized skills, Dr. Priebe became the founding chief of the Division of Pediatric Surgery.
At Stony Brook, Dr. Priebe developed a strong patient care service, and was recognized as a meticulous surgeon, tireless teacher, and a mentor of surgical faculty, residents, and medical students.
Now, with more than 3,000 outpatient visits and more than 1,000 surgeries annually, we have the largest pediatric surgery program in Suffolk County.
Longtime colleague Richard J. Scriven, MD, who worked closely with Dr. Priebe since 2001 when he joined our Pediatric Surgery Division, remembers: "Dr. Priebe was loved by his patients. For a complicated child, it was not unusual for him to spend hours with them on the ward or in the office.
"Dr. Priebe was a model for the next generation. He believed it was the highest honor for a parent to entrust their most precious gift to us for their surgical care."
During Dr. Priebe's academic career he had been active in research involving the causes of intestinal ischemia that may occur in premature newborn infants. His pediatric surgical interests focused on newborn congenital anomalies, pediatric tumors, and childhood trauma.
He always envisioned a hospital dedicated to caring for children that would further distinguish Stony Brook Medicine.
Dr. Priebe served on multiple national committees of pediatric surgical societies, and published articles on numerous pediatric surgical topics. Following his retirement from out full-time faculty, he continued to serve as an editorial consultant for the Journal of Pediatric Surgery, the leading journal in the field.
In 2010, to further support our mission of excellence in education, Dr. Priebe became the principal donor of the fund and leader of our campaign to establish the Cedric J. Priebe Jr., MD, Endowed Pediatric Surgery Lectureship.
The Priebe Lectureship fund now supports an annual visiting professor's presentation centering on a current clinical or research issue in pediatric surgery. This lecture presentation, given as part of our Surgical Grand Rounds program, focuses on new methods to improve patient care, as well as new research in the field of pediatric surgery.
This lectureship was one of Dr. Priebe's dreams — to help advance the education at Stony Brook of surgeons caring for children — and it remains part of his legacy in the Department of Surgery.
Beyond that, Dr. Priebe desired to have his legacy grow not only through the pediatric surgery lectureship but also through the creation of a dedicated children's hospital here at Stony Brook — a hospital just for kids that offers every clinical specialty and that would be competitive with similar hospitals throughout the country.
This dream of Dr. Priebe's has finally been realized. Stony Brook Children's Hospital is the first of its kind in Suffolk County, offering the most advanced pediatric specialty care in the region. It occupies two floors in the sparkling new Hospital Pavilion.
Our present chief of pediatric surgery Christopher S. Muratore, MD, adds: "Dr. Priebe really wanted to see the formal opening of our new Children's Hospital, which will take place in the near future but too late for him. He long thought a hospital dedicated to caring for children would be critical for our growth, expansion of services, and potential to optimize children- and family-centered healthcare."
| Visitation will be on Tuesday, January 22, 2019 from 2:00 to 4:00 pm and from 7:00 to 9:00 pm at the Bryant Funeral Home, 411 Old Town Road, East Setauket, NY. Funeral mass will be held on Wednesday, January 23, 2019, at 9:30 am at St. James RC Church, 429 Route 25A, East Setauket, NY. |
To honor Dr. Priebe and help ensure the longevity of the Priebe Lectureship, donations are encouraged. Make a gift to it online, or call the Stony Brook Medicine Advancement Office at 631-444-2899.
Posted by Stony Brook Surgery on January 16, 2019

| Dr. Aaron R. Sasson (left) and Dr. Georgios V. Georgakis |
Pancreatic cancer is the devastating cancer that over time took the lives of Luciano Pavarotti, Simone Signoret, Dizzy Gillespie, Patrick Swayze, Juliet Prowse, and Anne Francis. The images of the faces of these public figures toward the end of their lives tell what terrible tolls on the body this cancer brings about.
According to the American Cancer Society, about 55,440 people (29,200 men and 26,240 women) will be diagnosed with pancreatic cancer this year, and fewer than one in five of these cancers are caught early enough to be surgically removed.
Even when diagnosed early, pancreatic cancer typically spreads rapidly, and is seldom detected in its early stages. Signs and symptoms may not appear until the cancer is quite advanced.
For all stages of pancreatic cancer combined, the one-year relative survival rate is 20%, and the five-year rate is 8%.
Survival rates are low because fewer than 10% of patients' tumors are confined to the pancreas at the time of the diagnosis; in most cases, the malignancy has already progressed to the point where surgical removal is impossible.
At Stony Brook, we offer state-of-the-art diagnosis and treatment of pancreatic cancer, including innovative surgical options. In 2009, we pioneered the procedure called irreversible electroporation (IRE), which had never before been used for pancreatic cancer; specifically, the ablation (destruction) of pancreas tumors.
Since then, we have added new techniques that help patients in their quest for better cancer care, such as robotic pancreatic surgery. With the addition of our new state-of-the-art Cancer Center, we can provide our patients the best treatment options available internationally.
Here, our surgical oncologists Aaron R. Sasson, MD, and Georgios V. Georgakis, MD, PhD, both pancreas specialists with expertise in IRE, answer frequently asked questions about this new technology and its use in treating pancreatic cancer.
Q: What is IRE?
A: IRE is a surgical technique that kills the cancer by using electrical fields to generate pores in the tumor cells. It kills tumor cells without causing collateral damage to adjacent tissue. The NanoKnife, a computerized system used for the procedure, uses brief and controlled electrical impulses to open microscopic pores in a targeted area.
By increasing the number, strength, and duration of the electrical pulses, pores in the cells remain open permanently, causing microscopic damage. The cells then die, and the body rids itself of these dead cells.
IRE is very useful in treating complex tumors that involve vital structures, such as arteries and veins, that otherwise would not be able to be treated without sacrificing such structures.
The Stony Brook Cancer Center is the first center on Long Island to be
designated by the National Pancreas Foundation as a Pancreatic Cancer Center.
Q: What are the benefits of IRE?
A: IRE does not generate heat or cold, which could damage normal, adjacent tissues. For example, when a pancreatic cancer is deemed inoperable because it involves the artery that feeds the bowel, or the artery that supplies the liver, this tumor can be treated with IRE, and be destroyed. The main benefit of IRE is that it gives us the potential to offer treatment to some patients who previously had no options.
This breakthrough technology, however, is not viable for those patients where the cancer has metastasized, or spread elsewhere in the body. But, for those patients who are candidates, the procedure may result in a major improvement in quality of life and extended time beyond the anticipated few months associated with the advanced level of disease.
Q: Can IRE destroy an entire pancreas tumor?
A: IRE cannot destroy the tumor, in the same way that radical surgery does. IRE destroys the majority of the tumor, and it allows other modalities, such as chemotherapy, to have a better effect, prolonging patient survival effectively.
Q: Can IRE alone be used instead of conventional surgery to treat pancreatic cancer?
A: IRE can be used either along with conventional surgery, to maximize the potential of possible cure in patients whose tumors can be removed surgically, or it can be used alone in cases where the tumors cannot be removed. It cannot be used instead of conventional surgery.
Q: Has the safety of IRE ablation of pancreas tumors been established?
A: Yes, there are multiple published studies establishing the safety of IRE ablation of the pancreas in people.
Patients with pancreatic cancer who come to Stony Brook can be assured
they will receive the most sophisticated and compassionate care available today.
Q: How do patients tolerate the IRE procedure? Is it easy or hard to undergo?
A: IRE ablation for pancreatic tumors is applied surgically most of the times; that is, it needs a surgical procedure, either through small or big incision. Because there is nothing removed during these procedures, the recovery time is significantly shortened compared to the classic operations for pancreatic cancer.
Q: What are the side effects of IRE when used to treat pancreatic cancer?
A: The most common side effect is self-limiting pain. This pain typically lasts for a few days and passes without any major interventions. Other side effects can include pancreatitis, bleeding around the site of application, and leak of pancreatic or biliary juices.
Q: How long — in terms of years — has IRE treatment been shown to extend survival?
A: The median survival of patients who have been through IRE ablation of their inoperable tumors can be up to 27 months, according to published data.
Q: Is IRE for pancreatic cancer widely available?
A: Unfortunately, it is not. IRE is only available at select centers, including Stony Brook Cancer Center.
Q: What is the benefit of having IRE pancreas tumor ablation treatment at Stony Brook Cancer Center?
A: At Stony Brook Cancer Center, we provide world-class patient care from highly specialized doctors, using cutting-edge technology, in the heart of Long Island. We provide comprehensive diagnosis and multidisciplinary treatment for pancreatic cancer, and are leading the way in patient care.
Our center is designated by the National Pancreas Foundation (NPF) as a Pancreatic Cancer Center. It is the first NPF Cancer Center on Long Island. The NPF offers this distinction only to those institutions that treat the "whole patient" and that offer some of the best outcomes and improved quality of life for patients with pancreatic cancer.
Patients with pancreatic cancer who come to Stony Brook can be assured they will receive the most sophisticated and compassionate care available today, and that IRE may indeed be a life-extending option for them.
Posted by Stony Brook Surgery on January 9, 2019
Mediastinal tumors are benign or cancerous growths that form in the mediastinum; that is, the area in the middle of the chest between the sternum (breastbone) and spinal column.
The mediastinum, which separates the lungs, houses the heart, esophagus, trachea, great vessels, thymus, and lymph nodes.
Mediastinal tumors are relatively uncommon. They tend to be more common in young and middle-aged adults, but they may affect people of all ages.
These tumors develop in one of three areas of the mediastinum: the anterior (front), the middle, or the posterior (back). Different tumors are more common in certain age groups.
Children usually develop tumors in the back of the mediastinum, and they are often benign tumors. Adults usually develop them in the front, and these tumors can be cancerous.
Mediastinal tumors often pose a diagnostic and therapeutic challenge to thoracic surgeons. Surgical skill and experience, thus, are critical to successful treatment outcomes.
Here, Henry J. Tannous, MD, a specialist in mediastinal tumors and member of our Cardiothoracic Surgery Division, answers frequently asked questions about these tumors and their management.
Q: What causes mediastinal tumors to form?
A: Depending on etiology, a mediastinal tumor can be caused by an enlarged lymph node, or a gland such as the thymus, thyroid, or parathyroid. It can also be caused by a cyst originating from the pericardium (the sac that houses the heart), the bronchus, or the esophagus. Another cause of a mediastinal tumor can be a cancer that has spread into the mediastinum.
Q: How many different kinds of mediastinal tumors are there?
A: Mediastinal tumors can be classified by location (anterior, middle, and posterior) or by benign versus malignant. An anterior mass is the most common, and it could represent a thymoma, a lymphoma, a germ cell tumor, or a thyroid mass.
Q: What are the common mediastinal tumors?
A: Thymomas are the most common mediastinal tumors. They start in the thymus, which is a small organ in the front part of the chest under the breastbone. They represent one third of anterior mediastinal tumors and 15-20% of all tumors.
Thymomas could be associated with myasthenia gravis, which is a disease of the neuromuscular junctions causing weakness, and which is present in about half of all patients with thymoma at some stage.
Thymomas grow slowly and invade surrounding structures; consequently, these tumors require surgical removal with a good cure rate. A rarer but more invasive type, thymic carcinoma, is harder to manage and could require surgery, chemotherapy, and/or radiation.
Lymphomas are the second most common mediastinal tumor, and account for one fourth of all anterior mediastinal tumors. The most common types are Hodgkin lymphoma and B-cell lymphoma .
Q: What complications are associated with mediastinal tumors?
A: Complications of mediastinal tumors may include spinal cord compression (numbness, pain, weakness) and the spread of either benign or malignant tumors to nearby structures such as the heart and great vessels (aorta and vena cava).
Q: What are the symptoms of mediastinal tumors?
A: Sixty percent of patients with mediastinal tumors experience symptoms. These include cough, feeling of fullness in the chest, shortness of breath, substernal pain, and weight loss.
Other possible symptoms include fever/chills, night sweats, coughing up blood, swollen lymph nodes, respiratory blockage, and hoarseness.
At Stony Brook University Hospital, we provide leading-edge multidisciplinary care
to give all patients with mediastinal tumors the best possible outcomes.
Q: How are mediastinal tumors diagnosed?
A: A CT scan of the chest is the most commonly used imaging study to define the mediastinal tumor size and extension. Once the tumor mass is confirmed, a biopsy is usually indicated.
A CT-guided needle biopsy is occasionally possible and sufficient to make a diagnosis.
A cervical mediastinoscopy is another diagnostic technique. It consists of a small incision made at the base of the neck. It allows the visualization and biopsy of any growths around the airway (via direct vision or with the help of a miniature camera).
Other diagnostic surgeries include an endobronchial ultrasound-guided biopsy, or a thoracoscopic biopsy (usually excisional).
Q: How are mediastinal tumors treated?
A: Depending on the cause, a mediastinal tumor can be watched (an asymptomatic and non-enlarging cyst). Once a diagnosis is confirmed, the treatment can range from surgical removal (thymic tumors) to chemotherapy (lymphomas or germ cell tumors).
Q: What kind of surgery is used to treat them?
A: Once a decision is made to surgically remove a mediastinal tumor, there generally are two approaches that are used: an anterior approach done through a cut in the front of the chest and breastbone (sternum), called a sternotomy; or a lateral approach done through tiny incisions on the side of the chest, in between ribs, with a minimally invasive procedure called VATS.
VATS stands for video-assisted thoracoscopic surgery . A thoracoscope is a tiny video camera that transmits images of the inside of the chest onto a video monitor, guiding the surgeon in performing the procedure.
VATS might be performed with a surgical robot; that is, a high-tech instrument the surgeon may use to achieve the most precise surgery. Robotically-assisted VATS require not only the technology but special expertise on the part of the surgeon.
Our thoracic surgeons at Stony Brook Medicine use the latest technology,
and they have many years of experience in treating patients with mediastinal tumors.
Q: What are the risks of surgery for mediastinal tumors?
A: As with any surgery, there is always a small risk of bleeding or infection. However, due to the location of the mediastinal tumors, there is an extra layer of surgical complexity due to the proximity of vital structures such as the heart and esophagus that have to be preserved.
Q: What is the survival rate for patients with cancerous mediastinal tumors?
A: Most surgically removed mediastinal tumors have a favorable outcome. The kind of tumor, the stage, and the surgical margins status dictate the ultimate outcome. Non-surgical tumors like lymphomas also respond readily to chemotherapy.
Q: What is the advantage of having mediastinal tumors treated at Stony Brook Medicine?
A: At Stony Brook University Hospital, we provide leading-edge multidisciplinary care to give patients with mediastinal tumors the best possible outcomes. Our surgeons use the latest technology, and have many years of experience in treating patients with these tumors.
Patients can undergo video-assisted thoracoscopic surgery (VATS) for the removal of mediastinal tumors. This approach uses small incisions, and provides faster recovery than traditional procedures that require large incisions and opening the chest.
If the tumor is more extensive or potentially invading vascular structures, a sternotomy (incision in middle of chest) or hemi-sternotomy (incision in upper half of chest) is commonly used.
Rarely, the removal of the tumor requires placing the patient on cardiopulmonary bypass — a procedure used for open heart surgery to temporarily bypass the heart function — to allow for a more aggressive surgery to take out the tumor.
In less sophisticated hospitals without bypass machines, these tumors would be deemed inoperable and, instead of surgery, patients would be treated with chemotherapy or radiation. Such an approach may be less than ideal because surgery has been shown to provide the best outcomes.
Posted by Stony Brook Surgery on January 7, 2019
New Access to Our Vascular Care Benefits Patients on South Shore
| Our vascular specialists at Long Island Community Hospital: (l to r) Drs. Mohsen Bannazadeh, Pamela S. Kim, and Nicholas Sikalas. |
We are very pleased to announce that our Vascular and Endovascular Surgery Division is now offering its diverse clinical services in Patchogue at Long Island Community Hospital.
This clinical relationship with Long Island Community Hospital will benefit the growing South Shore community, and comes just a year after the start of a similar relationship with our trauma services.
Our vascular team provides diagnostic and therapeutic services for the entire spectrum of vascular disorders. Our surgeons perform a wide array of open and endovascular procedures for management of arterial and venous diseases. They have special expertise in:
- Open and endovascular repair of aortic aneurysms and aortic dissections
- Surgery and stenting for stroke prevention (carotid endarterectomy; carotid stenting; transcarotid artery revascularization)
- Treatment of peripheral arterial disease (PAD) with open and minimally invasive techniques
- Repair of traumatic arterial and venous injuries
- Surgery for diabetic foot ulcers
- Open and endovascular procedures for hemodialysis access
- Minimally invasive surgery for varicose veins and venous obstruction
About the addition of our vascular services at Long Island Community Hospital, Richard T. Margulis, president and chief executive officer there, says:
"We couldn't be more proud to work with these incredible physicians who will be helping us to expand the services we offer to the community. Our top priority is always the serving community and offering this new life-saving care without the delay of transfer is a benefit that is beyond measurement."
Stony Brook Surgical Associates is now offering in Patchogue at Long Island Community Hospital
a scope of diagnostic and treatment options for vascular care unique in Suffolk County.
Apostolos K. Tassiopoulos, MD, professor of surgery, vice chair for quality and outcomes, and chief of our Vascular and Endovascular Surgery Division, says:
"Our goal is to bring the most sophisticated vascular care closer to patients. By expanding our practice to Long Island Community Hospital, we will provide easier access to the latest and most advanced vascular and endovascular therapies for patients living on the South Shore, and will enhance the cardiology and trauma services currently offered there."
Our program in minimally invasive endovascular surgery offers a broad scope of diagnostic and treatment options which are unique in Suffolk County. Our team of nationally and internationally recognized expert physicians will now be providing daily these state-of–the-art services in the Patchogue area.
As part of our vascular services, patients in Long Island Community Hospital will also have access to the services of our Center for Vein Care, which is fully accredited by the Intersocietal Accreditation Commission. Our vein care specialists provide treatment for:
- Acute deep vein thrombosis
- Chronic venous thrombosis
- Pelvic congestion syndrome
- Varicose and spider veins
- Venous ulcerations
Our specialists use the latest surgical and non-surgical techniques to treat varicose veins and spider veins of the leg, including new minimally invasive "endovenous" techniques that let patients get back to their normal activities in usually just a couple of days. No general anesthesia or hospitalization is required.
Our vascular surgeons have been recognized for many years for their clinical excellence by selection for inclusion in the Castle Connolly Guide, Top Doctors: New York Metro Area, representing the top 10% of physicians in the New York Metropolitan area.
Patients can be seen at our Patchogue office, which is just across the street from Long Island Community Hospital, at 100 Hospital Road, Suite 203 (map/directions).
Posted by Stony Brook Surgery on January 2, 2019
Our Thyroid Specialists Use a Multidisciplinary Approach to Managing Thyroid Disorders
An estimated 20 million Americans suffer from a thyroid disorder, and many more go undiagnosed every year. Now is a good time to become aware of your thyroid and its relationship to your health — and how best to take care of it.
Thyroid nodules and enlarged thyroid glands are common problems, and they can harbor cancers within them. They require proper evaluation and treatment.
When detected, patients with these thyroid disorders are usually referred for further work-up to an endocrinologist, or to an experienced head and neck surgeon, like one of the head and neck surgeons at Stony Brook Medicine.
January is national Thyroid Awareness Month that aims to bring to the public's attention the need to take good care of this important tiny gland in the neck.
Following a thorough work-up, the patient may need to undergo thyroidectomy (removal of part or all of the thyroid gland) for several reasons — for removal of thyroid cancer, removal of part of the thyroid gland for definitive diagnosis, treatment of a hyperactive thyroid gland, or an enlarged thyroid gland that is causing breathing or swallowing difficulties.
The thyroid gland is a small, butterfly-shaped gland located in the base of the neck just below the Adam's apple. Although relatively small, the thyroid gland influences the function of many of the body’s most important organs, including the heart, brain, liver, kidneys, and skin. Ensuring that the thyroid gland is healthy and functioning properly is important to the body's overall well-being.
Surgical intervention is the gold standard in thyroid cancer; there are no other options to cure it.
Since thyroid cancers are highly curable, it is extremely important for the patient to undergo proper treatment and close follow-up. The initial treatment for most thyroid cancers is removal of the thyroid gland, and sometimes removal of lymph nodes which may contain metastatic cancer.
In the hands of a highly-skilled, experienced surgeon, the procedure can usually be done on an outpatient basis and with a low risk of complications. Depending on the type of cancer, some patients may require treatment with radioactive iodine after surgery.
| Our thyroid specialists, (l to r) Drs. Lukasz Czerwonka, Melissa M. Mortensen, and Ghassan J. Samara. |
Also essential is close follow-up by the patient's endocrinologist for tumor surveillance and regulation of the thyroid hormone.
Our thyroid specialists take a multidisciplinary approach to providing care for patients with thyroid disorders. The team of physicians consists of surgeons, endocrinologists, radiation oncologists, radiologists, and pathologists.
Management decisions are often made jointly among the team members. Such a team approach has ensured long-term successful outcomes for our patients at Stony Brook Medicine.
Hyperthyroidism is a sustained overly active thyroid gland, which may result in anxiety, nervousness, rapid heartbeat, weight loss, and high blood pressure. The causes of hyperthyroidism include Grave's disease and toxic nodular goiter. This condition is treated with medications, radioactive iodine, or thyroidectomy.
The advantage of surgery is that the condition can be treated quickly and effectively, minimizing the risk of recurrence. In the past, non-surgical treatment has been the primary approach to patient care because of potential complications associated with the surgery. Now, with surgical expertise and advances in technology at Stony Brook Medicine, more patients are undergoing surgery with minimal complications.
In the past, goiter was treated with medication, but that was proved not to be effective. Patients with goiter now have surgery to alleviate the pressure symptoms on the trachea and the esophagus.
Thyroidectomy is performed for nodules and cancer of the thyroid gland. It is also performed in some patients with overactive thyroid glands.
Stony Brook Medicine provides patients state-of-the-art thyroid care using the multidisciplinary team approach, distinguished by highly experienced surgical specialists capable of treating all forms of thyroid conditions.
| The thyroid gland is a small, butterfly-shaped gland located in the base of the neck just below the Adam's apple. Although relatively small, the thyroid gland influences the function of many of the body’s most important organs, including the heart, brain, liver, kidneys, and skin. The blue paisley ribbon icon is the universal symbol of thyroid disease awareness and advocacy. Paisley was chosen because it resembles a cross-section of thyroid follicles, the tiny spheres that the thyroid gland is made of. |
Perform the do-it-yourself thyroid neck check. Watch this video (1:00 min) about thyroid awareness from the American Association of Clinical Endocrinologists:
Posted by Stony Brook Surgery on January 1, 2019
Williams Demonstrates the Poetic Can Be Found Everywhere around Us
"January Morning" is one of the most famous poems by America's great physician-poet William Carlos Williams (1883–1963). A masterpiece of modernist verse, this poetic sequence — he subtitled it "Suite" — presents moments in his daily life, including his life as a pediatrician and obstetrican at Passaic General Hospital in Passaic, NJ.
The poem first appeared in Williams's book, Al Que Quiere! (1917; "To Him Who Wants It!"; Centennial Edition published from New Directions). His voice in it remains totally vibrant. The New York Review of Books recently said, "It seems clear that Williams is the 20th-century poet who has done most to influence our very conception of what poetry should do."
The young doctor is dancing with happiness / in the sparkling wind, alone / at the prow of the ferry!
"January Morning" demonstrates beautifully Williams's poetic method using concrete images, which he later summarized in the phrase "No ideas but in things." His command of language in his verse made him a leader of the modernist revolution against the popular sentimental poetry using vague abstractions. Indeed, it was a revolution against the poetry his friend Ezra Pound said "flies away into the circumambient gas." Williams's poetry is grounded in the world around us.
Williams lived his entire life in Rutherford, NJ, the small town where he was born and raised. It is where he maintained his medical office in his home — where most people knew him simply as "Doc" without knowing he was a man of letters and leader of modernism. He often spent time in Manhattan with fellow artists, crossing the Hudson River by ferry. Al Que Quiere! was his third book but the first to present his unique poetic voice, as found in "January Morning."
All told, Williams published during his lifetime some 20 books of poetry as well as 17 books of prose, including novels, and he delivered more than 3,000 babies. Throughout his career he used his clinical gaze to his advantage as a poet:
|
I I have discovered that most of the beauties of travel are due to the strange hours we keep to see them: the domes of the Church of the Paulist Fathers in Weehawken against a smoky dawn—the heart stirred— are beautiful as Saint Peters approached after years of anticipation. II Though the operation was postponed I saw the tall probationers* in their tan uniforms hurrying to breakfast! III —and from basement entries neatly coiffed, middle aged gentlemen with orderly moustaches and well-brushed coats IV —and the sun, dipping into the avenues streaking the tops of the irregular red houselets, and the gay shadows dropping and dropping. V —and a young horse with a green bed-quilt on his withers shaking his head: bared teeth and nozzle high in the air! VI —and a semicircle of dirt-colored men about a fire bursting from an old ash can, VII —and the worn, blue car rails (like the sky!) gleaming among the cobbles! VIII —and the rickety ferry-boat "Arden"! What an object to be called "Arden" among the great piers,—on the ever new river! "Put me a Touchstone at the wheel, white gulls, and we'll follow the ghost of the Half Moon to the North West Passage—and through! (at Albany!) for all that!" IX Exquisite brown waves—long circlets of silver moving over you! enough with crumbling ice crusts among you! The sky has come down to you, lighter than tiny bubbles, face to face with you! His spirit is a white gull with delicate pink feet and a snowy breast for you to hold to your lips delicately! |
X The young doctor is dancing with happiness in the sparkling wind, alone at the prow of the ferry! He notices the curdy barnacles and broken ice crusts left at the slip's base by the low tide and thinks of summer and green shell-crusted ledges among the emerald eel-grass! XI Who knows the Palisades as I do knows the river breaks east from them above the city—but they continue south —under the sky—to bear a crest of little peering houses that brighten with dawn behind the moody water-loving giants of Manhattan. XII Long yellow rushes bending above the white snow patches; purple and gold ribbon of the distant wood: what an angle you make with each other as you lie there in contemplation. XIII Work hard all your young days and they'll find you too, some morning staring up under your chiffonier at its warped bass-wood bottom and your soul— out! —among the little sparrows behind the shutter. XIV —and the flapping flags are at half-mast for the dead admiral. XV All this— was for you, old woman.† I wanted to write a poem that you would understand. For what good is it to me if you can't understand it? But you got to try hard— But— Well, you know how the young girls run giggling on Park Avenue‡ after dark when they ought to be home in bed? Well, that's the way it is with me somehow. |
* Nursing students.
† WCW's mother, who rejected his modernist poetry.
‡ Street in Rutherford, NJ, near WCW's home.
|
William Carlos Williams practiced pediatrics and obstetrics for over 40 years. He was a physician of immense integrity, who regarded
allegiance to humanism as important as excellence in medical science. He now serves as a role model, and medical students read him
(The Doctor Stories) to learn how he
labored to get the "right picture" of patients — much like artists do with paint on canvas, and photographers with cameras; what
today we call the holistic approach. At Stony Brook Medicine, Williams is read in The Center for Medical Humanities, Compassionate Care, and Bioethics. Established in 2008 to expand and succeed the Institute for Medicine in Contemporary Society, the Center is dedicated to furthering the School of Medicine's long tradition of emphasizing humanism in medical education, and serving as "a place where the human side of medicine is elevated, examined, and revered." |
Listen to Allen Ginsberg (4:16 min), whom Williams mentored, reading from and commenting on "January Morning." For more biographical info, see our post Remembering William Carlos Williams."