| Volume 29 Number 3 | Stony Brook, NY | < March 2018 > |
 |
|
|
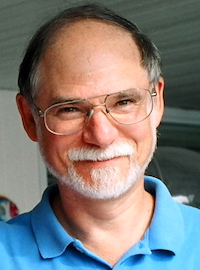
Dr. Joshua Dubnau - Professor

Dr. Joshua Dubnau has been officially appointed as Professor of Anesthesiology. Josh arrived in August 2016 after having spent much of his career working at Cold Spring Harbor Labs. He has a lively and productive NIH-funded lab in the Center for Molecular Medicine Building on the West Campus. Visit his lab web pages for details (and great pictures) about his research on Amyotrophic Lateral Sclerosis and Frontotemporal Lobar Degeneration using his favorite organism - the fruitfly. For the last eight months, Josh has been serving as the Chairman of the Research Committee of the department. Congratulations, Josh! 
|
March Calendar

The daffodil is the flower of March.
Wed. Mar 7. Dr. TJ Gan will chair the Faculty Meeting at 7:00 am in Lecture Hall 5.
Thurs. Mar 8. Journal Club will meet at the Eastern Pavillion in Setauket from 6:00 - 8:00 pm. The discussion topic is "Deliberate Hypotension". See the Journal Club web page for details. Wed. Mar 14. Dr. Joshua Miller from the Department of Medicine will present a Faculty Grand Rounds talk at 7:00 am in Lecture Hall 5. Dr. Miller is the Medical Director of Diabetes Care for Stony Brook Medicine and an Assistant Professor of Endocrinology & Metabolism in the Department of Medicine. He is dual board-certified in Internal Medicine and Endocrinology, Diabetes & Metabolism. His main area of clinical research is the relationship between diabetes and colon cancer. Wed. Mar 21. Dr. Richard Thalappillil will present his Senior Grand Rounds talk at 7:00 am in Lecture Hall 5. 
|
|
Medical Mission to Ecuador
Ruchir Gupta, MD 
We learned how to improvise, at one point even doing general anesthesia cases 
We want to thank Dr. TJ Gan and the Anesthesia Department for sponsoring this trip. This experience helps physicians like us truly give back to society and find ways to intertwine our own practice down the road to include volunteer work. We hope this experience remains intact for future residents. View the photo album from this mission. 
|
|
OB Epidural Video
Justin Smith, MD

We started by creating a survey to assess patient’s understanding of epidurals and also their experience receiving an epidural during their hospital stay. Then, we developed a short script and vision for what we would like the video to include. After our script and storyboard were completed, we found a videographer to come and shoot and edit the video. It was fun and educational working with the videographer as he taught us what would work best for the different segments we wanted to produce. The CA-3 class acted as narrators, patients, nurses, and family members to complete the video. Working with the media relations staff for the hospital, we now have a finished video which we are going to start showing to patients prior to labor. We hope that patients will have the opportunity to view the video when they come for tours of the obstetric suite and in some clinical situations prior to coming to the hospital in labor. The video is posted on the Stony Brook OB anesthesia patient information website for all to see. We plan to follow up with another survey after patients have seen the video to see if patient satisfaction and understanding of epidurals improves after seeing the video. Looking back on the experience so far, we realize the importance of being very particular about what is scripted and how we want the different segments to be staged. Putting some more thought into the specifics of the story board would have made the day we spent making the video go more smoothly. Also, getting media relations involved earlier in the process would have been a great aid in developing this video since they had a lot of great recommendations that we could have incorporated earlier in the planning process. Overall, making this video has been very enjoyable and educational. We look forward to continuing this project over the next few months. 
|
|
Meeting Report - Cutting Edge Topics in Pediatric Anesthesia
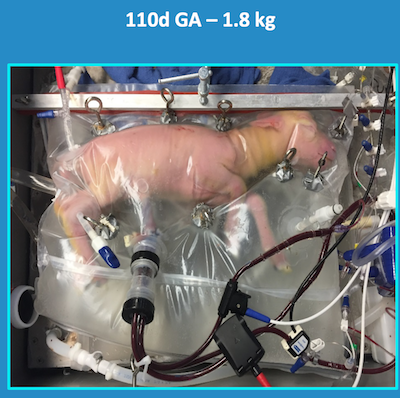
Ronald Jasiewicz, DO, MBA, FAAP This winter I was the New York invitee to "Cutting Edge Topics in Pediatric Anesthesia", a Philadelphia Pediatric Anesthesiology consortium meeting. The keynote speaker, Alan Flake MD, a pediatric CHOP surgeon/researcher, presented a glimpse of the potential for the human artificial placenta. Flake reiterated that the pulmonary system takes the biggest hit with premature births. In simplicity, "no ventilation modality when studied by RCT has reduced death or BPD in extreme premature infants." Current ventilation strategies include a myriad of approaches ranging from nCPAP to HFOV, have not had significant impact. The issue is an arrest of lung development due to gas ventilation in the extra-uterine environment. 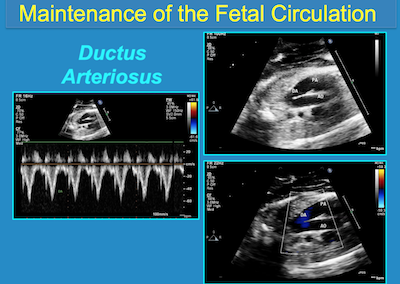

In brief, the EXTEND animal model had normal: oxygen parameters, somatic growth and maturation, lung development and maturation, and brain growth and maturation.

When the question arose during the Q&A: Who will manage these fetuses in Biobags? The consensus from the surgeon and the audience of pediatric anesthesiologists was unanimously ... the neonatologists! Aysha Hasan M.D. was also present and sends her regards to all. As you may not know, Aysha left the SB Anesthesiology Pediatric Team to pursue a Pediatric Regional Anesthesia Fellowship at Boston Children's. The Monday following the meeting she commenced her new position as Director of the Acute Pain Service at St. Christopher's Children's hospital in Philadelphia. She is proudly expecting her first child this March! 
|
|
New Publications


|
|
Where on Campus is That?
James P. Dilger, PhD 
(And, what was I doing on the roof of the Chemistry Building?) 
|
|
Monthly Muscle Chillaxant


|
|
Erratum
In the February 2018 issue of SleepTalker we inadvertently gave the wrong name for Megan Lindstadt's husband. The newlyweds are Megan Lindstadt and John Felsberg! We regret the error; it has been corrected in the online version of the newsletter. We wish Megan and John much happiness in their future together!

|
|
SleepTalker, the Stony Brook Anesthesiology Newsletter is published by the Department of Anesthesiology
Stony Brook Medicine, Stony Brook, NY Tong Joo Gan, M.D., M.H.S., F.R.C.A., M.B.A., Chairman Editorial Board: James P. Dilger, Ph.D.; Stephen A. Vitkun, M.D., M.B.A., Ph.D.; Marisa Barone-Citrano, M.A.; Richard Tenure, M.D. |