
| Volume 34 Number 3 | Stony Brook, NY | < September 2020 > |
 |
 |
| PJ Poppers Memorial | STARS | Kudos | SASM Meeting |
| Family News | Alumni News | CA-3 Resident Spotlight! | Peek Behind the Publication |
| CRNA News | New Publications | Photography Corner | Where on Campus is That? |
|
Paul J. Poppers Memorial Lectureship
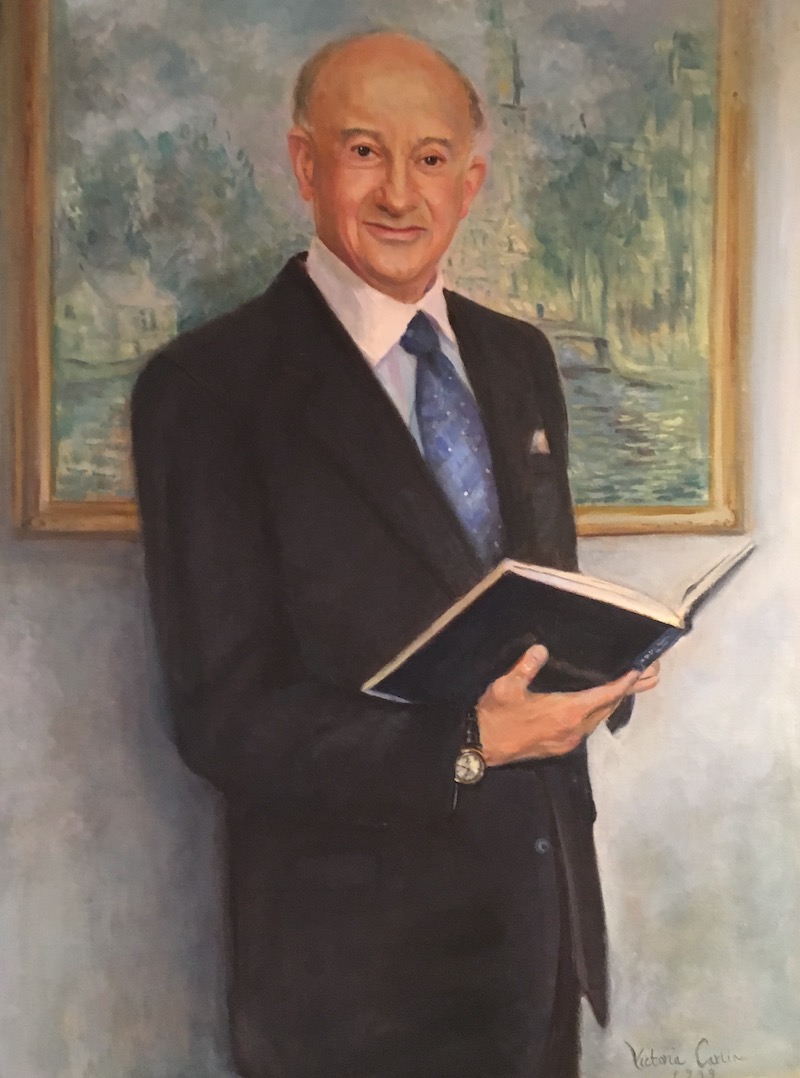
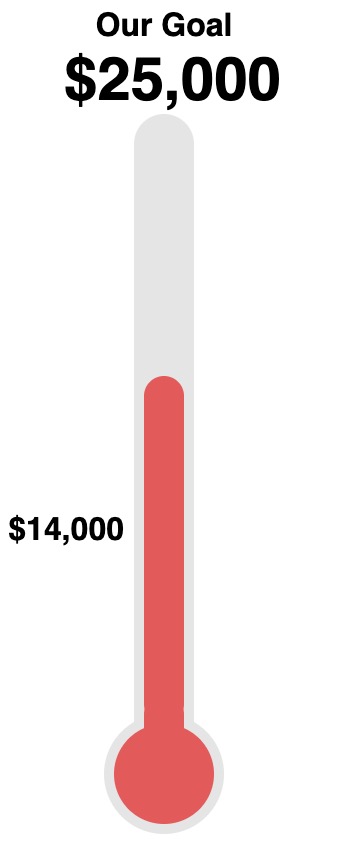
Our department and the family of Dr. Paul Poppers intend to honor the memory of our founding chairman by establishing an endowed lectureship, which will enable the department to invite a renowned guest speaker each year to deliver the Paul J. Poppers Distinguished Lecture. This fund is administered through the Stony Brook Foundation and is established in perpetuity. Fundraising was on a hiatus during the past few months. Now that things have settled down, we are moving forward again. Our goal is to raise a minimum of $25,000 from our colleagues in addition to the $50,000 contributed by the Poppers family and our own Department. We were actually doing quite well moving towards our goal, having raised about $14,000 at the end of March when I temporarily suspended the process. We invite you to participate with a gift of your own toward the fund. All donations are welcome. Whatever you choose to give, please know that the amount of your donation will never be shared with either the department or the family. Use this link, type "poppers" in the search box, and select "The Paul J Poppers, MD Distinguished Visiting Endowed Lectureship in Anesthesiology". Thank you!  |
|
Kudos
 Dr. Duran Mitchell wrote a Residents' Review "Living #BlackLivesMatter in Medicine" for the August 2020 issue of the ASA Monitor.
Dr. Duran Mitchell wrote a Residents' Review "Living #BlackLivesMatter in Medicine" for the August 2020 issue of the ASA Monitor.He was also invited to serve as a member on 2020 HOD Reference Committee on Professional Affairs at the Oct 3 virtual House of Delegates meeting. Congratulations! 
|


Dr. Jamie Lee Romeiser completed her PhD program in Population Health and Clinical Outcomes Research. She has now been hired by the department as a Data Manager/Statistician. Congratulations!  |
|
2020 Society of Anesthesia and Sleep Medicine Meeting
 Dr. Sergio Bergese and his colleagues will present two abstracts at virtual SASM meeting to be held October 1-2, 2020.
Dr. Sergio Bergese and his colleagues will present two abstracts at virtual SASM meeting to be held October 1-2, 2020.• Driver CN, Laporta ML, Bergese SD, Urman RD, Di Piazza F, Sprung J, Weingarten TN. Temporal Distribution of Postoperative Respiratory Depression • Laporta ML, Driver CN, Bergese SD, Urman RD, Di Piazza F, Sprung J, Weingarten TN. PRODIGY Risk Assessment Score and Frequency of Opioid-Induced Respiratory Depression  |
|
Family News
 Ursula Landman, DO
Ursula Landman, DO
Our daughter, Sarah, graduated from Comsewogue High School and is beginning her Freshman year at SUNY Binghamton studying Premed and majoring in Biochemistry. Matthew begins his senior year at SUNY Albany and continues to study Japanese. He hopes to travel to Japan for his final semester. William is in the writers room for the show "Raised by Wolves" starting September 3 on the HBOMax streaming service. Ira and I are very proud of all of them!  |
|
New Publications
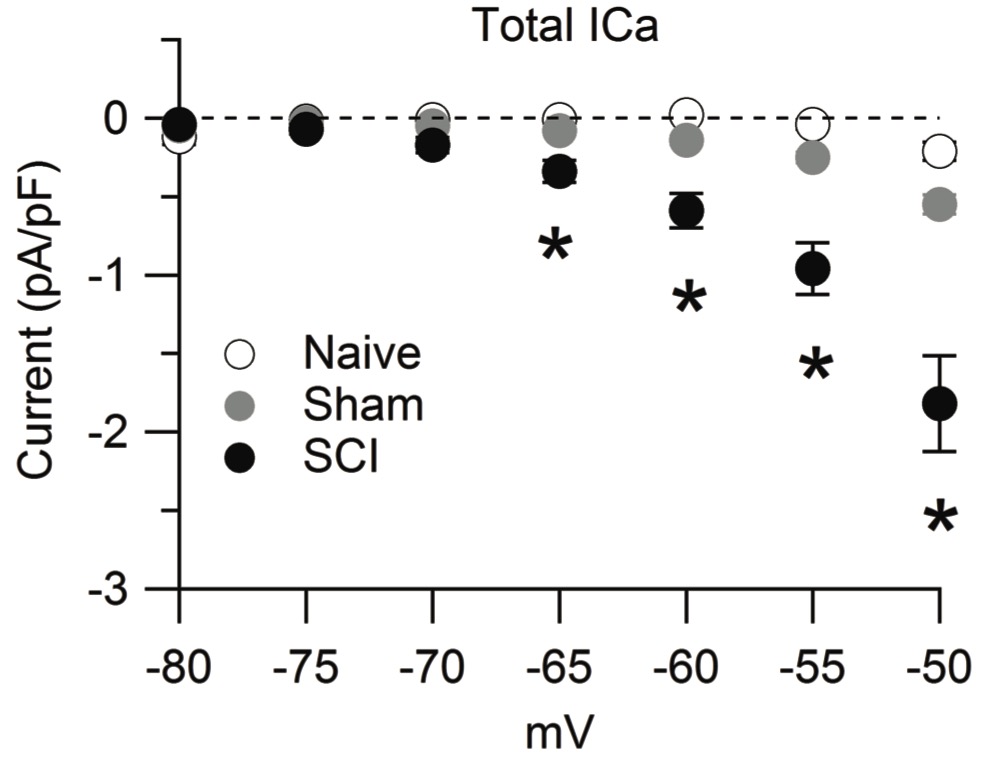 Figure from Lauzadis et al 2020
 |
|
Photography Corner
Kathleen Dilger, MS 

|
|
Where on Campus is That?
|
|
SleepTalker, the Stony Brook Anesthesiology Newsletter is published by the Department of Anesthesiology
Stony Brook Medicine, Stony Brook, NY Tong Joo Gan, M.D., MHS, FRCA, MBA, Chairman Editorial Board: James P. Dilger, Ph.D.; Stephen A. Vitkun, M.D., M.B.A., Ph.D.; Marisa Barone-Citrano, M.A.; Ramanjot S. Kang, M.D. |





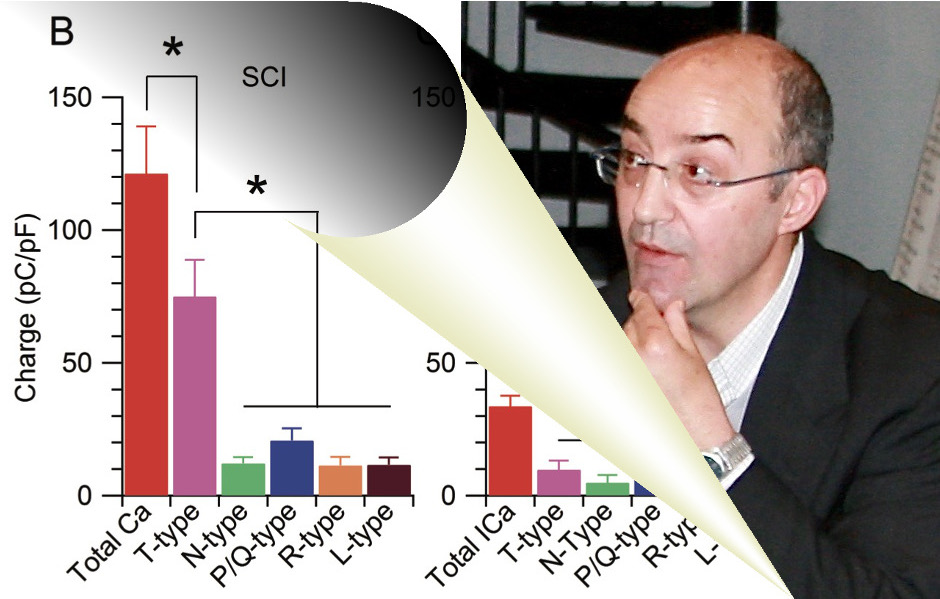 Chronic neuropathic pain is a major comorbidity of spinal cord injury (SCI), affecting up to 70-80% of patients. SCI-induced neuropathic pain (SCI-pain) is often lifelong and therapeutically intractable, resulting in severe decline of quality of life and increased risks for depression, anxiety, and addiction.
Chronic neuropathic pain is a major comorbidity of spinal cord injury (SCI), affecting up to 70-80% of patients. SCI-induced neuropathic pain (SCI-pain) is often lifelong and therapeutically intractable, resulting in severe decline of quality of life and increased risks for depression, anxiety, and addiction.  Delirium is a highly distressing postoperative complication associated with significant morbidity and mortality. With the ever-increasing number of older patients undergoing major surgeries, delirium management will likely become even more relevant to everyday practice. As there are currently very limited treatment options available for established delirium, I undertook this project to find out what can be done in the perioperative setting to minimize the risk of delirium, and what areas require further studies.
Delirium is a highly distressing postoperative complication associated with significant morbidity and mortality. With the ever-increasing number of older patients undergoing major surgeries, delirium management will likely become even more relevant to everyday practice. As there are currently very limited treatment options available for established delirium, I undertook this project to find out what can be done in the perioperative setting to minimize the risk of delirium, and what areas require further studies.